Research & Publications > The Hong Kong Practitioner > Clinical Quiz

Clinical Quiz (Please login 'Member Area' for online submission of latest issue)
Clinical Quiz June 2025
A 66-year-old lady with newly diagnosed diabetes mellitus developed itchy papules and nodules over legs for 2 months
Dr. Adrian KC Cheng
|
Readers are invited to participate in the Clinical Quiz*. Simply answer the question, fill in the reply slip and return it to the College by 21 August 2025. Each reader is allowed to submit one entry only.
*Note: There would be no prize award for this issue while sponsorship for Clinical Quiz has been ended in September 2020 issue. The answer of the Clinical Quiz for this issue will be announced in the next issue. Thank you for your support.
|
Clinical history:
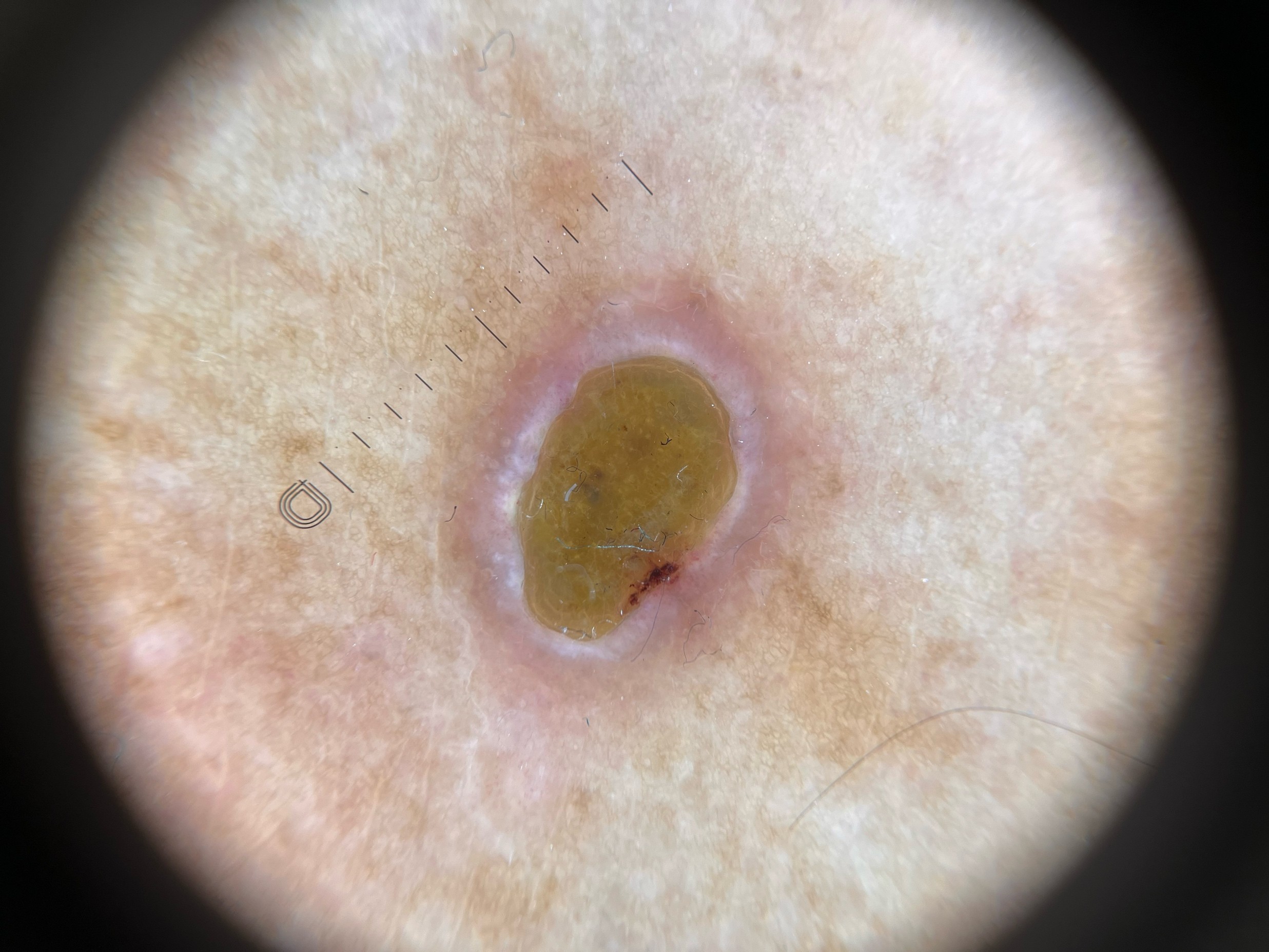
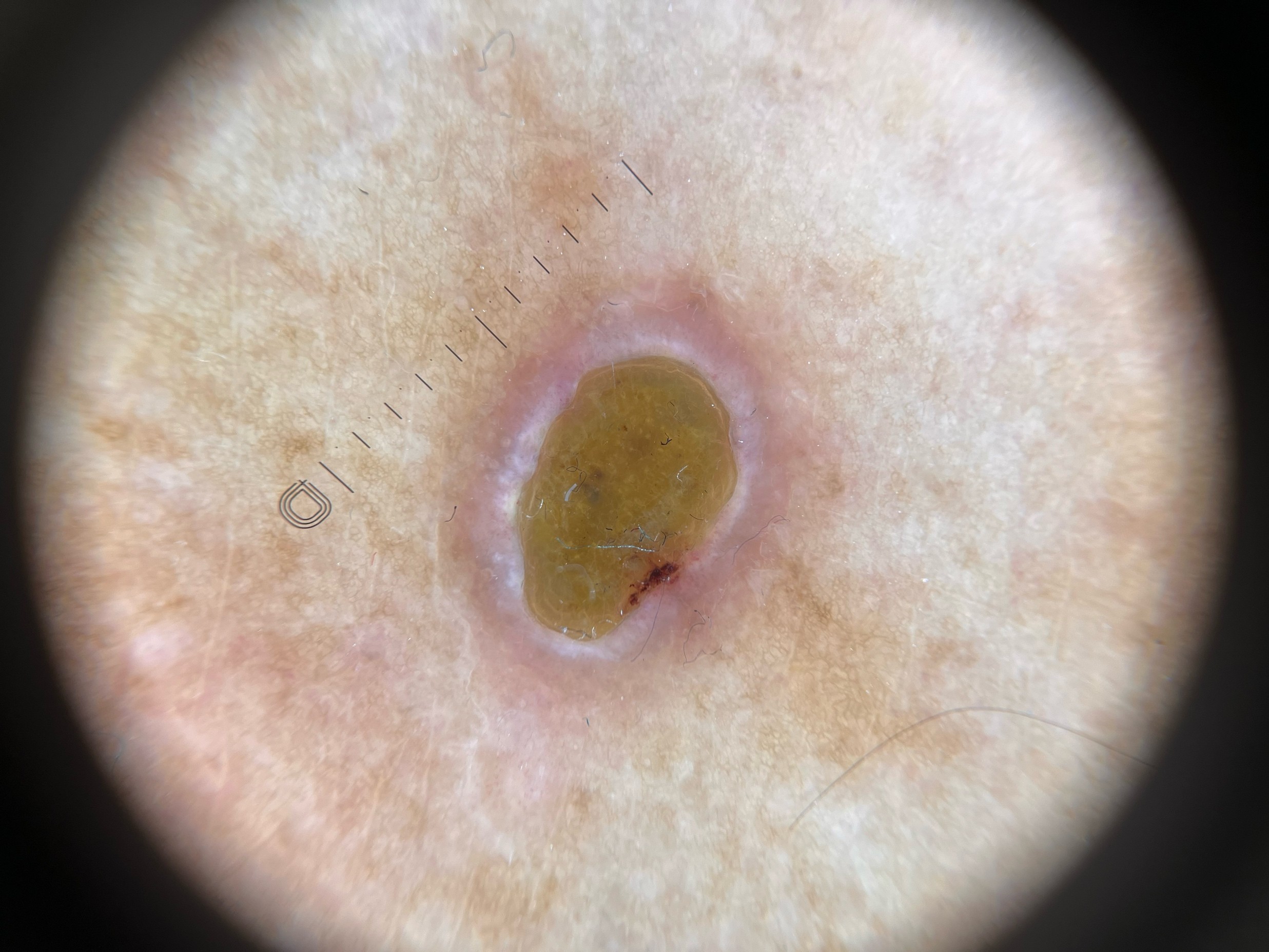
A 66-year-old lady with a history of psoriasis and newly diagnosed diabetes mellitus developed these itchy papules and nodules over her legs for 2 months. Examination showed multiple papules and nodules with a raised erythematous rim, surrounding erythema with central keratin plugging. There were post-inflammatory hyperpigmentation on her legs resulting from previous psoriatic plaques. Dermoscopic view of the nodules showed a central hyperkeratotic plug with an elevated erythematous rim. HbA1c was 12%.
What is the diagnosis?


| A. | Prurigo nodularis |
| B. | Acquired perforating dermatosis |
| C. | Disseminated keratoacanthoma |
| D. | Erythema multiforme |
Answer:
B. Acquired perforating dermatosis
Acquired perforating dermatosis (APD) classically presents in adults with chronic renal failure or diabetes mellitus, often in association with poorly controlled glycaemia. The exact pathogenesis is uncertain. It is thought to involve transepidermal elimination of dermal connective tissue, triggered by microtrauma, pruritus, and microangiopathy related to diabetes.
Clinically, APD manifests as intensely pruritic papules and nodules, usually distributed over the extensor surfaces of the lower limbs, though the trunk and upper extremities may also be affected. Lesions characteristically show a raised erythematous border with a central keratotic plug. The post-inflammatory hyperpigmented patches over the legs were a result from previous psoriatic plaques.
Dermoscopy further supports the diagnosis, with the finding of a central hyperkeratotic plug surrounded by an erythematous rim, correlating with the histological hallmark of transepidermal elimination of collagen and elastin fibres. The markedly elevated HbA1c (12%) suggests poorly controlled diabetes, a recognised precipitating factor for APD.
Skin biopsy showed an umbilicated lesion, with a central plug composed of parakeratotic debris, degenerative collagen, and inflammatory cells. The epidermis deep to the plug is markedly thinned or ulcerated, and is traversed by vertically orientated collagen fibers. Thses findings are consistent with acquired perforating dermatosis.
The main differential diagnoses include prurigo nodularis, hypertrophic lichen planus, perforating folliculitis, and keratoacanthoma; however, the clinical morphology and dermoscopic findings in this case are in keeping with APD.
Management involves optimisation of the underlying systemic disease, particularly improving glycaemic control. Symptomatic treatment includes topical corticosteroids, keratolytics, and emollients to reduce pruritus and scaling. Phototherapy (narrowband UVB), systemic retinoids, or allopurinol may be considered for refractory disease.
The slide and the question were prepared by:
Dr. Adrian KC Cheng, MBBS(HK), MRCP(UK), MSc GEOR (CUHK), FHKCP, FHKAM (Medicine)
Specialist in Dermatology & Venereology;
Associate Consultant,
Division of Dermatology, Department of Medicine, Queen Mary Hospital, Hong Kong SAR
Back