Research & Publications > The Hong Kong Practitioner > Clinical Quiz

Clinical Quiz (Please login 'Member Area' for online submission of latest issue)
Clinical Quiz December 2022
An 80-year-old man presented with a pigmented lesion over the left
frontotemporal scalp for many years
Sze-man Wong, Ka-chun Cheng
|
Readers are invited to participate in the Clinical Quiz*. Simply answer the question, fill in the reply slip and return it to the College by 16 February 2023. Each reader is allowed to submit one entry only. The name of the winner and the answer will be published in the March 2023 issue.
*Note: There would be no prize award for this issue while sponsorship for Clinical Quiz has been ended in September 2020 issue. The answer of the Clinical Quiz for this issue will be announced in the next issue. Thank you for your support.
|
Clinical history:
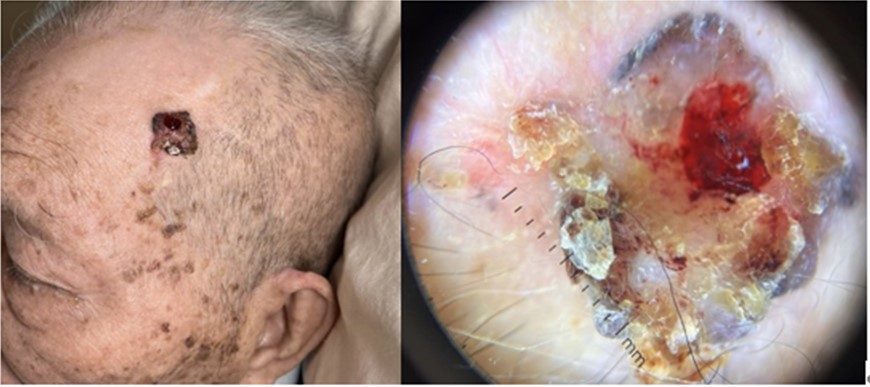
An 80-year-old man presented with a pigmented lesion over the left
frontotemporal scalp for many years. He noted that the lesion was not
bothersome except that it might occasionally bleed when he scratched it.
What is the diagnosis?
| A. | Basal cell carcinoma |
| B. | Squamous cell carcinoma |
| C. | Malignant melanoma |
| D. | Irritated seborrheic keratosis |
Answer:
A. Basal cell carcinoma
There are three major types of skin cancers—basal cell carcinoma, squamous cell carcinoma and melanoma. Basal cell carcinoma (BCC) is the most common type of skin cancer, constituting about 90% of all skin cancers in Hong Kong. The incidence rate of BCC in HK has increased by one-third from 2009 to 2019.1 In 2019, there were 1081 new cases of non-melanoma skin cancer, accounting for 3.1% of all new cancer cases in Hong Kong. The crude annual incidence rate of non-melanoma skin cancer per 100 000 Hong Kong population was 14.
BCC is also known as rodent ulcer, which is locally invasive. Patients with BCC often develop multiple primary tumours over time. It usually occurs in people over 40 years. Since about 50% of people with BCC developed a second one within three years, they are at an increased risk of other skin cancers such as melanomas, hence regular self-skin examinations and referral for dermatologist skin checks are advised. BCCs are particularly prevalent in elderly males. However, they also affect females and younger adults. Previous BCC and other forms of skin cancers such as squamous cell carcinoma and melanoma, sun damage such as photoaging, prior episodes of sunburn, fair skin types, exposure to arsenic, and immune suppression due to disease or medicine are well-known risk factors for the development of BCCs.
In this elderly man, who was a retired policeman and had a fair skin type, he had several sun damage signs over his face, such as multiple seborrheic keratosis and solar lentigos. He presented with nodular type BCC, which has a shiny or pearly smooth surface and central depression or ulcerations, with the edges appearing to be raised and rolled, so call ‘roll-up ‘edge, while blood vessels crossed
the surface with arborising branches as shown in the dermoscopic view on the right.
The cause of BCC is multifactorial. There are DNA mutations in the patched PTCH tumour suppressor gene part of the hedgehog signalling pathway. These may be triggered by exposure to ultraviolet radiation or various spontaneous or inherited gene defects predisposing to the development of BCC. The BCC is locally invasive with a characteristically slow growing nature, presented as a nodule or plaque with skin coloured, pink or pigmented, and spontaneous bleeding or ulceration. They vary in size, starting from a few millimetres to several centimetres in diameter. As in this case, it was neglected by the patient, and the lesion slowly increased in size with bleeding and ulcerations. There are several clinical subtypes of BCCs and over 20 histological growth patterns. The nodular BCC
is the most common type of facial BCC. Superficial basal cell carcinoma is the most common type in younger adults and appears most often on the upper trunk and shoulders.
BCC can be diagnosed clinically, and the histological subtype is usually confirmed pathologically by a skin biopsy.
The treatment2 of a BCC depends on its type, size and location as well as patient factors. Most BCCs are treated surgically with a 3-5mm margin of normal skin around the tumour. Imiquimod cream is an immune response modifier which is best used for superficial BCCs less than 2cm diameter, usually resulting in variable inflammatory reaction, and scarring. Radiotherapy can be used as adjunctive treatment if margins are incomplete. It is mainly used if surgery is not suitable. Targeted therapy such as hedgehog signalling pathway inhibitors, e.g. vismodegib,can be considered in those locally advanced primary, recurrent or metastatic BCCs. Long-term follow-up is recommended to check for new lesions and recurrence.
In this man, nodular BCC was confirmed. He was referred to surgery for complete excision with a
clear margin and possible skin grafting. Alternatively, radiotherapy may be considered as primary or adjuvant treatment considering the advanced age in this case. It isworth noting that skin cancer is often neglected by the elderly, and it is essential for clinicians to recognise this important skin condition and refer for early treatment.
References
1. Common cancers In Hong Kong, The cancer online resource Hub, The government of Hong Kong SAR.
https://www.cancer.gov.hk/en/hong_kong_cancer/common_cancers_in_hong_kong/skin_cancer.html (last access 10 October 2022).
2. Kim JYS, Kozlow JH et al. Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol. 2018 Mar;78(3):540-559. doi: 10.1016/j.jaad.2017.10.006
The slide and the question were prepared by:
Dr Sze-man Wong, MBBS(HK), MRCP(UK), MSc (London), FHKCP, FHKAM(
Medicine), FRCP (Edin)
Specialist in Dermatology and Venereology
Consultant,
Division of Dermatology, Department of Medicine, Queen Mary Hospital, Hong Kong SAR.
Dr Ka-chun Cheng, MBBS(HK), MRCP(UK), FHKCP, FHKAM ( Medicine)
Specialist in Geriatric Medicine
Associate Consultant,
Department of Medicine, Queen Mary Hospital, Hong Kong SAR.
Back