Supporting dying in place in Hong Kong –
Retrospective analysis of a cohort of terminally
ill patients in public sector with a preference
for dying at home
Jeffrey SC Ng 吳常青, Pui-chi Chiu 趙佩芝, Po-tin Lam 林寶鈿, Ka-yee Lee 李家儀, Kai-ming Li 李啟明
HK Pract 2021;43:80-88
Summary
Introduction:
The prevalence of dying at home in Hong
Kong is extremely low. A cross-specialty multidisciplinary
program supporting dying at home was established
since 2011 in a cluster of regional public hospitals.
Objective:
This study aimed to review the profile of
patients in the program, to explore factors favouring
home death, interventions delivered at home, reasons for
admission for hospital death and events after home death.
Methods:
patients who joined the programme before
2019 were included. Information was searched through
the electronic medical records of Hospital Authority
Results:
53 patients were recruited, of median age 81
(range 29 - 102), 66% female and 50.7% with cancer
diagnoses. Most (96.2%) patients had family caregiver(s)
and 49.1% also had foreign domestic helper (FDH).
Thirty-two patients (60.4%) achieved home death.
Factors favouring home death included having FDH
(62.5% and 28.6%, p = 0.016), nursing visits ≥ 5 times
per week (71.9% and 42.9%, p = 0.035) and having less
emergency admission and admission to palliative care (PC)
wards in the programme (3.1% and 28.6%, p = 0.012;
3.1% and 23.8%, p = 0.031). Interventions at home
covered symptom control, psycho-spiritual support and
caregiver education. Having refractory symptoms was the
main reason (85.7%) for hospital death. For patients who
died at home, 87.5% (28/32) received cardio-pulmonary
resuscitation (CPR) by emergency rescue personnel (ERP)
upon transfer to hospital.
Conclusions:
Dying-at-home is achievable in Hong
Kong. Presence of professional support at home is an
important determinant. Legal barrier resulting in futile
CPR by ERP against patient’s wish is yet to overcome.
摘要
導言:
香港的居家離世率極低。從2011年起,一組地區公立醫院設立了一項支持居家離世的跨專業多學科專案。
目的:
本研究旨在對專案患者的基本情況進行梳理,探討居家離世的有利因素、可在家開展的介入措施、在醫院離世的原因以及居家離世後的事件。
方法:
納入了2019年之前加入本專案的患者。資訊通過檢索醫院管理局的電子病歷獲得。
結果:
共納入了53名患者,年齡中位數81歲(29歲–102歲),女性佔66%,癌症患者佔50.7%。大多數患者(96.2%)有家人照護,49.1%的患者還有外籍家庭傭工照護。三分之二的患者(60.4%)實現了居家離世。有利於居家離世的因素包括:聘用外籍家庭傭工(62.5%和28.6%,p = 0.016),護士家訪≥每週5次(71.9%和42.9%,p = 0.035),以及在專案中較少入住急症和紓緩治療病房(3.1%和28.6%,p = 0.012;3.1%和23.8%,p = 0.031)。在家中開展的介入措施包括症狀管理、心理精神支持以及照護者教育培訓。在醫院離世的主要原因為有難治性症狀(85.7%)。在居家離世的患者中,87.5% (28/32)在轉運至醫院的途中接受過緊急救援人員的心肺復甦術。
結論:
居家離世在香港是可以實現的。在家中提供專業支援是重要的決定因素之一。因法律障礙而導致緊急救援人員違背患者意願進行無效心肺復甦術的情況尚待克服。
Introduction
An important element of End-Of-Life Care (EOLC)
is to let people with terminal illness to receive care
and to die in their preferred place. The percentage of
people being able to die in place has been proposed to
be an element of good death1
and a quality indicator
in palliative care/ EOLC in some countries.2
Family
satisfaction with EOLC is also strongly associated
with their relatives dying in their preferred place.3
Among different locations of death, home is commonly
acknowledged as the preferred place.4
Dying peacefully
in one’s bed at home has also been recognised as a
blessing in traditional Chinese belief.5
About 90% of Hong Kong (HK) people died
in government hospitals6
, but a recent HK survey
suggested that 31.2% of general public chose home
to be the preferred place of death.7
The preference for
home death may decrease with progression of illness8
,
consistent with local findings that only 13-19% of
patients receiving palliative care preferred to die at
home.9,10 Nonetheless, an earlier study in HK reported
extremely low prevalence – only 6 in 1300 cancer
patients died at home as preferred.11 Barriers for dying
at home in HK are multifold, including the inadequate
care available at home, the lack of community
professional support as well as the legal and logistic
concern after home death.12
As an attempt to support care-in-place and
dying-in-place, a cross-specialty multidisciplinary
programme has been established in regional public
hospitals in Kowloon East Cluster (KEC) of Hospital
Authority (HA) since July 2011. This dying-at-home
programme consists two parts: 1. care-in-place until
death supported by a community professional team
with expertise in palliative care and 2. dying-in-place
facilitated by verification of death in the Accident and
Emergency Department (AED).
The professional support at home is provided by
the KEC Virtual Ward service, which aims to deliver
“hospital-at-home” to patients with high risk of hospital
admissions13 and was found to be effective in reducing
unplanned emergency medical readmissions and in
improving the quality of life in frail older patients
after discharge.14 Terminally ill patients are prone to
repeated hospital admissions and are one of the targeted
service recipients of this service. With collaboration
with community nursing service, community support
up to daily home visit can be arranged as needed. The
service provides on-site medical and nursing support at
home and enquiry hotline from 9am to 5pm on Monday
to Sunday. Clinical admission to PC ward could be
arranged so as to avoid AED attendance. Team members
consist of community nurses, a specialist palliative care
(PC) nurse, a PC physician and a geriatrician.
The verification of death after a patient passed
away at home was smoothed out by a workflow
established between AED and PC team. This workflow,
which is named “Palliative Care Last Journey”, ensures
that the Certificate of the Cause of Death (Form 18)
would be issued to the patient who died in AED, such
that the deceased body would not be sent to public
mortuary as a reportable death.15 The AED is informed
beforehand of the list of patients recruited in the dying-at-home program. Recruited
patients would be given a
letter with attention to AED stating patient’s terminal
illness and the preference for dying at home and
refusal of cardio-pulmonary resuscitation (CPR). The
standardised HA Advance Directives (AD) forms16 (if
the patient is mentally competent) and Do-Not-Attempt
Cardio-Pulmonary Resuscitation (DNACPR) forms for
non-hospitalised patients (implemented since October
2014)17 would be signed in the programme. CPR would
be avoided in AED when patients were transferred
from home after death. The patient would be certified
dead by the AED doctors and the last office would be
performed by the AED nurses. The body is retained in
the hospital mortuary and the Certificate of the Cause
of Death (Form 18) would be completed by the PC
physicians.
People with advanced diseases receiving palliative
care service were referred for the dying-at-home
program. The criteria for enrolment are: (i) a clearly
stated preference for dying at home, (ii) such preference
accepted by the family and/or caregivers, (iii) having
at least one full-time caregiver and (iv) living in the
catchment area of United Christian Hospital (UCH) (later
extended to Tseung Kwan O Hospital in mid-2018).Patients with difficult symptom control
or inadequate
support from caregivers would be excluded upon initial
assessment. Since the establishment of this programme,
a significant portion of recruited patients have achieved
dying at home.
Objectives
This retrospective study would analyse the profiles
of the cohort of patients recruited into the dying-at-home programme. By comparing the
characteristics of
the subjects who died at home with those in hospital,
this study attempts to identify factors associated with
the place of death. This study will also explore the
interventions delivered during terminal care at home,
the reasons for final admissions in those who died in
hospital as well as the events after home death.
Methods
It is a retrospective cohort study. Patients who are
terminally ill and have been recruited in the above-mentioned dying-at-home programme
before 2019 and
living in UCH catchment area will be included in this
study. There is no exclusion criterion.
Information on patient’s place of death and data
on patient’s profile are extracted by review of the
electronic medical records of HA by the investigators.
Data collected are based on conceptual models
on determinants of place of death in systematic
reviews18,19, which include individual factors (including
demographics, patient’s preference), social factors
(including household members, characteristics of
caregiver, housing and social assistance), disease
factors (including diagnosis, functional status and
symptom profiles) and health care factors (including
care interventions at home and healthcare utilisation).
Functional status is assessed by using Palliative
Performance Scales (PPS) in this study. PPS uses five
observer-rated parameters (ambulation, activity and
evidence of disease, self-care, intake, and level of
consciousness). It is a reliable and valid tool and PPS
score has been found to be a strong predictor of survival
in patients receiving palliative care.20,21 Relatives' Stress
Scale (RSS) is used to measures caregiving stress of
family caregivers. It is a validated self-rated 15-item
scale with total score ranging 0 to 60 and score </= 23
suggesting low risk, > 30 suggesting high risk.22,23
Information on intervention in terminal care and
communication with patient and caregivers at home are
also based on documentation in the electronic medical
records. For the reasons of the last admissions in those
who died in hospital and the events after patients dying
at home, including any CPR by emergency rescue
personnel (ERP) or in AED, body being sent to public
mortuary and referral to coroner, they are retrieved
from AED records with supplemented information from
community nurses in dying-at-home programme.
The Statistical Package for the Social Sciences (SPSS)
version 21 is used for statistical analysis. Descriptive
statistics will be used to summarise the patient's health
conditions, socio-demographic characteristics and
treatments/ interventions received after recruitment into
the dying-at-home programme until death. Normality in
continuous variables is assessed by Kolmogorov-Smirnov
Test. Comparison between the two cohorts (those dying at
home and those in wards) will be done by Pearson Chi-square (or Fisher’s exact test
(FET) if the sample value
is less than 5) and Mann–Whitney U test. A significance
level with a p value < 0.05 will be used for all analyses.
This study received the approval from Kowloon
East Cluster/ Kowloon Central Cluster Research Ethics
Committee, HA (Reference number: KC/KE-18-0180/
ER-1).
Result
Totally 53 patients were enrolled in the dying-at-home program in the period from Jul
2011 to Nov
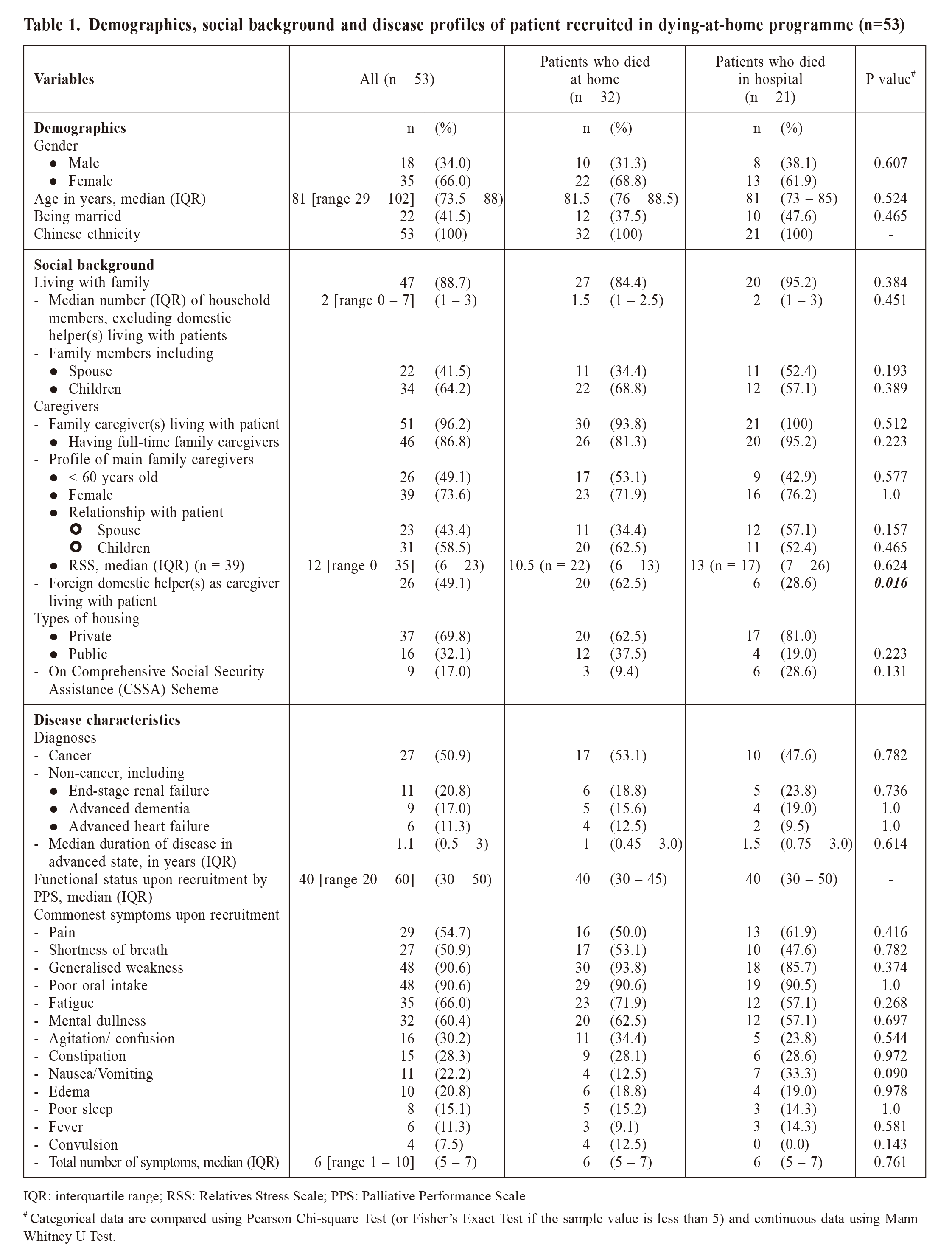
2018 and were all included in this study. Table 1
summarises the information on patient demographics,
social background and disease characteristics. Most
patients (96.2%) had full-time family caregivers and
nearly half (49.1%) had foreign domestic helpers
(FDH) as caregivers living with patients. The overall
caregiver stress by RSS was low with median score
of 12 (Interquartile range (IQR) 6 – 23), as score ≤
23 suggesting low risk.22,23 Half of the patients had
cancer diagnosis, including colorectal 8 (29.6%), lung
6 (22.2%), liver 3 (11.1%), breast 3 (11.1%) and other
types 7 (25.9%) of malignancy. Functional state was
poor with PPS of median 40, i.e. mainly in bed, unable
to do most activities and mainly requiring assistance in
self-care. The median number of symptoms were 6 (IQR
5 – 7), with generalised weakness and poor oral intake
being the most prevalent (in >90% of patients).
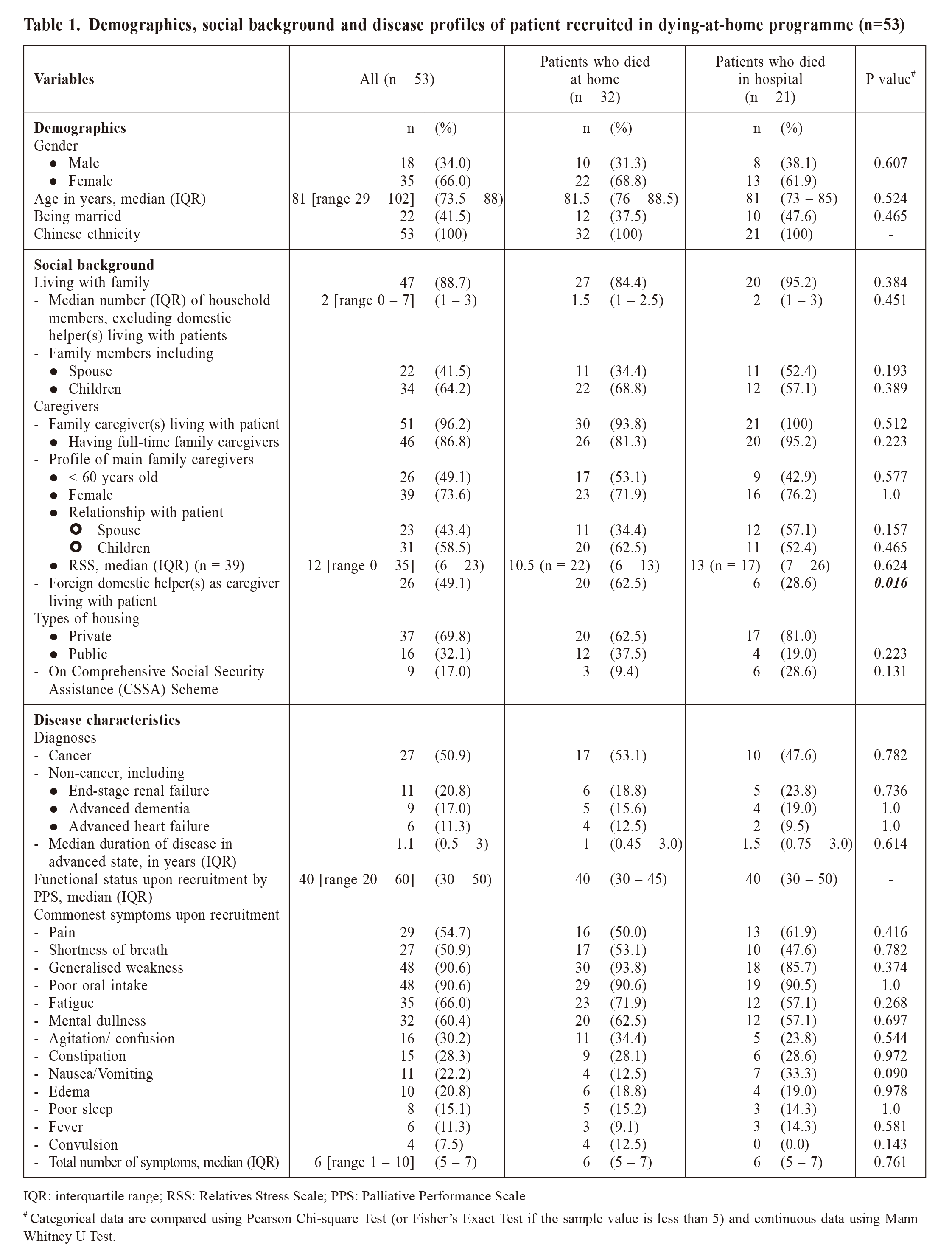
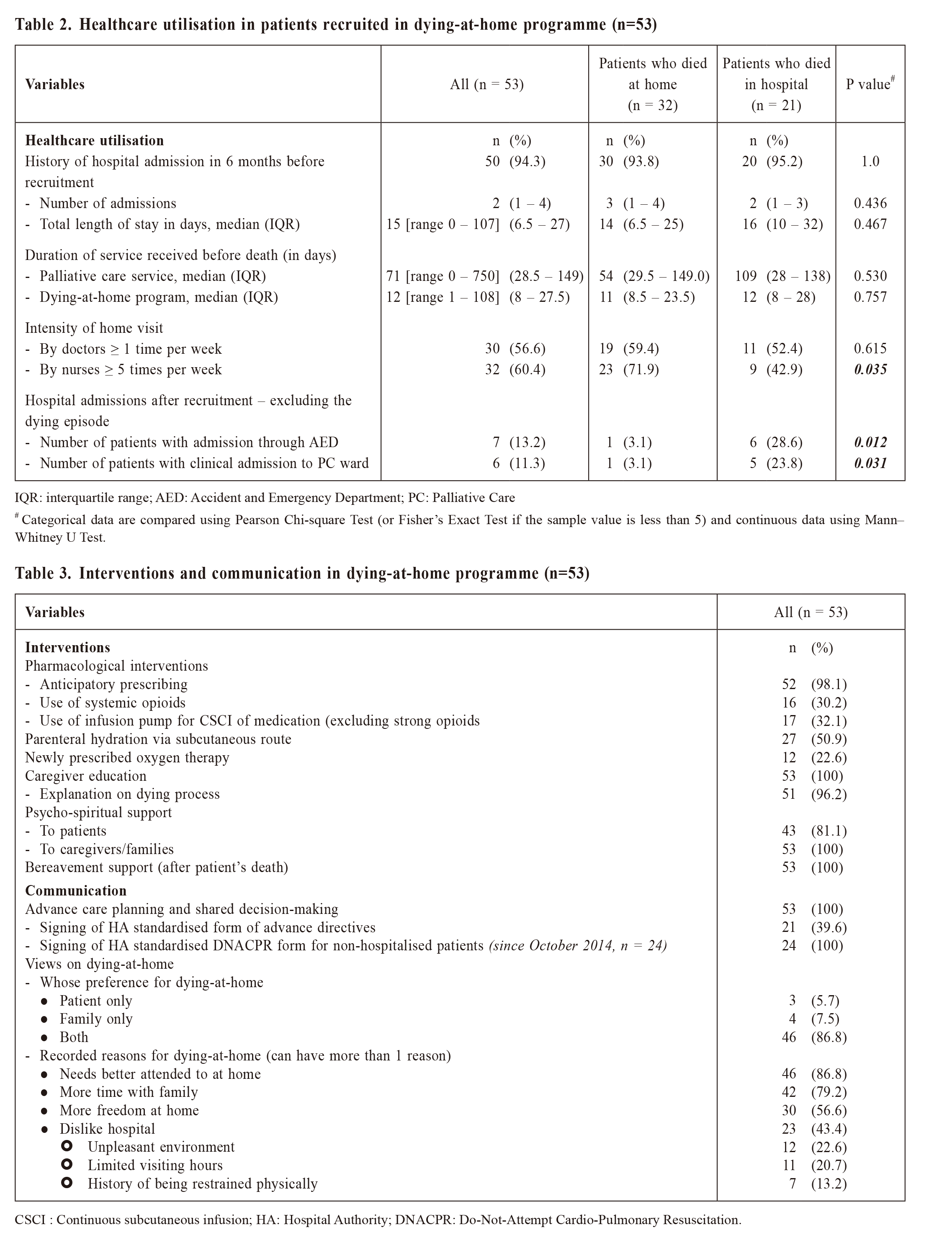
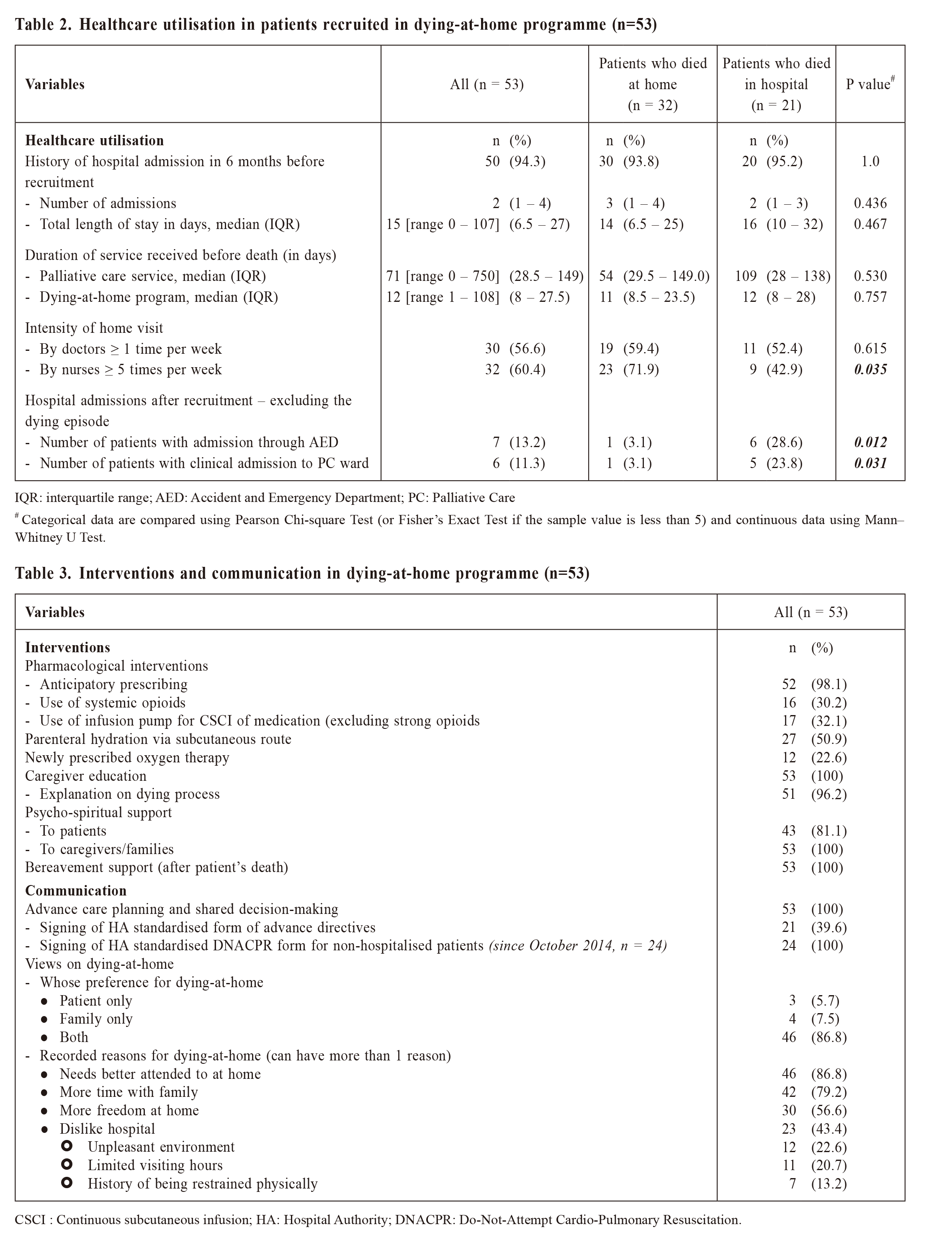
Table 2 shows the healthcare utilisation in patients
recruited in dying-at-home program. Most (94.3%)
patients had hospitalisation in the 6 months before
recruitment. Median duration of joining the dying-at-home program was 12 days (IQR 8 –
27.5 days). More
than half of the patients received doctor home visit
once or more per week and nursing home visit 5 times
or more per week within the programme. Around 10%
of patients still had hospitalisation despite intensive
support during the dying-at-home programme.
Thirty-two patients (60.4%) in the dying-at-home
programme achieved home death and the rest (39.6%)
died in hospital. Comparing those who died at home
with those in hospital, factors favouring home death
included having FDH as caregiver living with patient
(62.5% and 28.6% respectively, p = 0.016, FET),
received nursing visits ≥ 5 times per week (71.9% and
42.9%, X2
= 4.463, df = 1, p = 0.035) and having less
emergency admission and admission to PC wards during
the programme (3.1% vs. 28.6%, p = 0.012, FET,
and 3.1% and 23.8%, p = 0.031, FET, respectively).
Other demographic, social, disease and health care
variables are not found to have a statistically significant
association with the place of death.
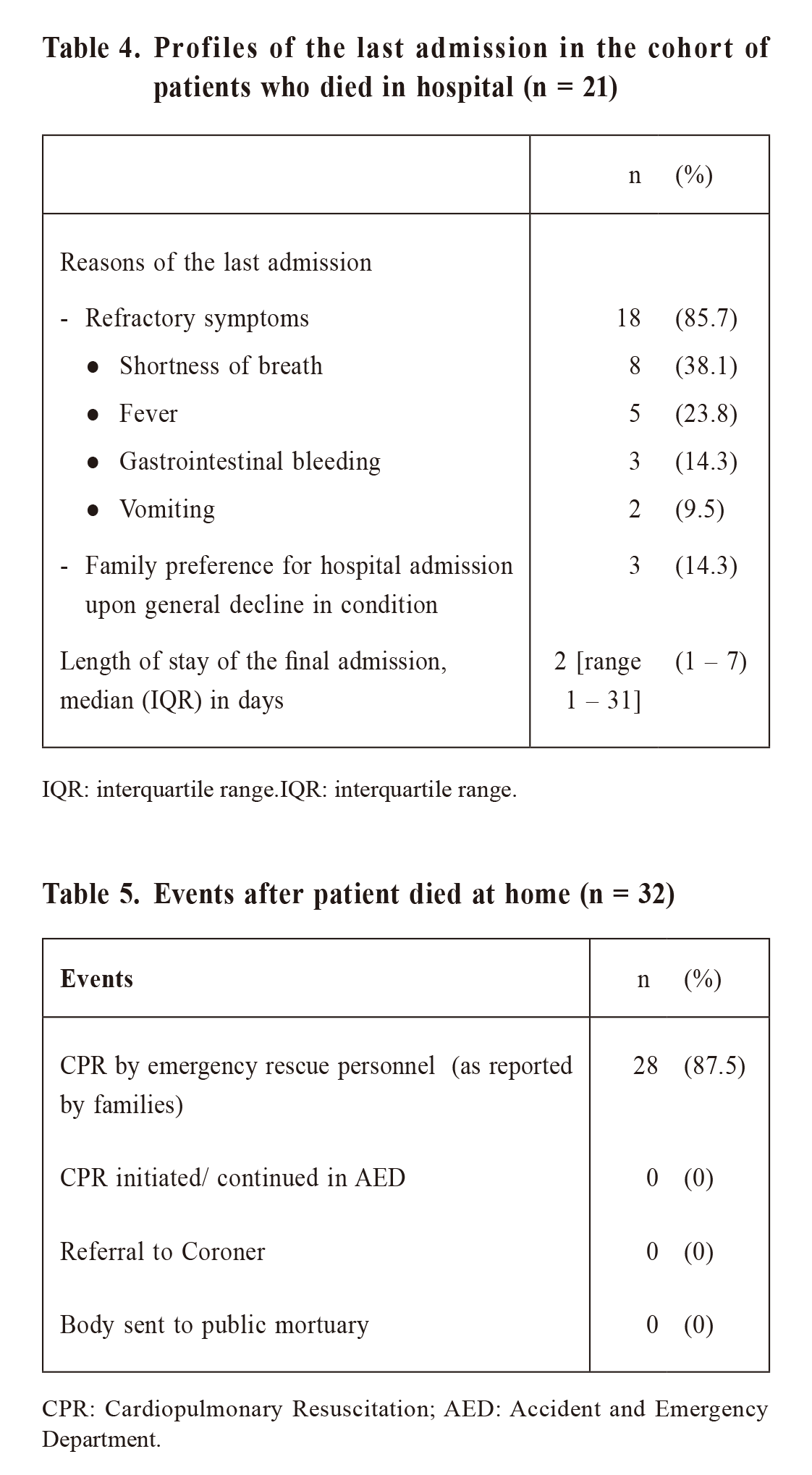
Table 3 shows the interventions and communication
in the dying-at-home programme. All except one patient
who died upon the first doctor visit had received
anticipatory prescription for symptom management.
Around 30% of patients used systemic opioids, including
tramadol (oral/ subcutaneous injection/infusion),
morphine (oral) and fentanyl (as transdermal patch).
One third of patients required continuous subcutaneous
infusion (CSCI) of medication, which included tramadol,
haloperidol, metoclopramide, hyoscine butylbromide
and furosemide. No strong opioids were administered
via CSCI route. Caregiver education was delivered
in all cases, which included symptom management,
use of medications, skills in bodily care as well as
explanation on signs of dying, potential catastrophic
events and practical procedures after home death. All
caregivers/ families received psycho-spiritual support
and bereavement care from community nurses in dying-at-home programme and from the
multidisciplinary
PC team. Advance care planning was reviewed in all
patients and HA standardised DNACPR forms for non-hospitalized patients were signed in
all after its rolling
out in October 2014. For the recorded reasons for
choosing home death, more than half mentioned that
their needs were better attended and there was more
time with family and more freedom at home. There is
no statistically significant difference identified in the
items listed in Table 3 between patients who died at
home and those in hospital.
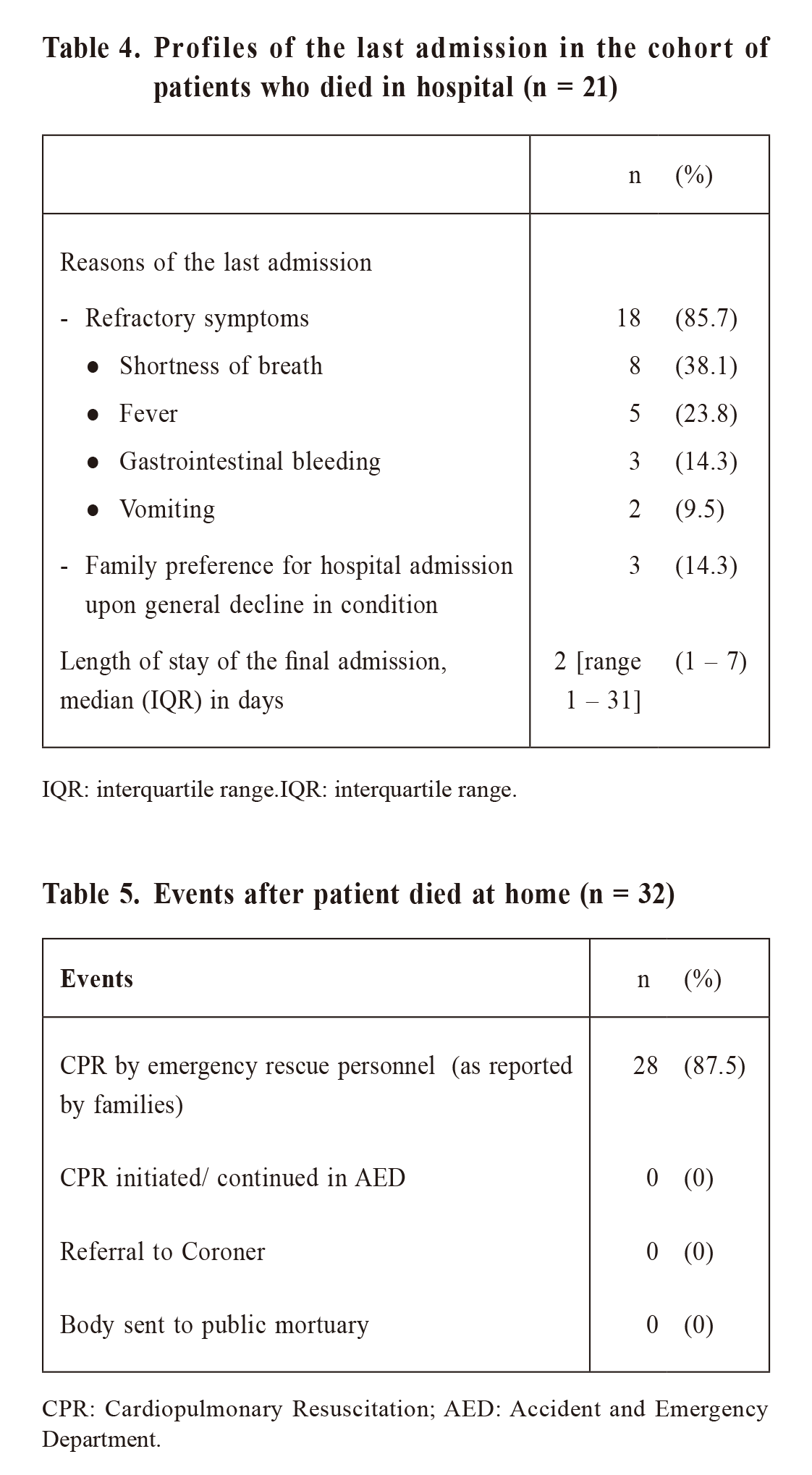
Among the patients who died in hospital, majority
(85.7%) was admitted for refractory physical symptoms
in which shortness of breath being the most common
(38.1%) (Table 4). In 3 (14.3%) patients, families
changed mind and preferred dying in hospital when
patients' condition further declined.
Table 5 shows the events in the cohort of patients
who died at home. Despite the presence of documents stating the preference against CPR,
families of 28
(87.5%) patients reported that CPR was performed by
ERP before arrival to AED. CPR was not initiated or
continued in AED. There was no referral to Coroner or
body being sent to public mortuary.
Discussion
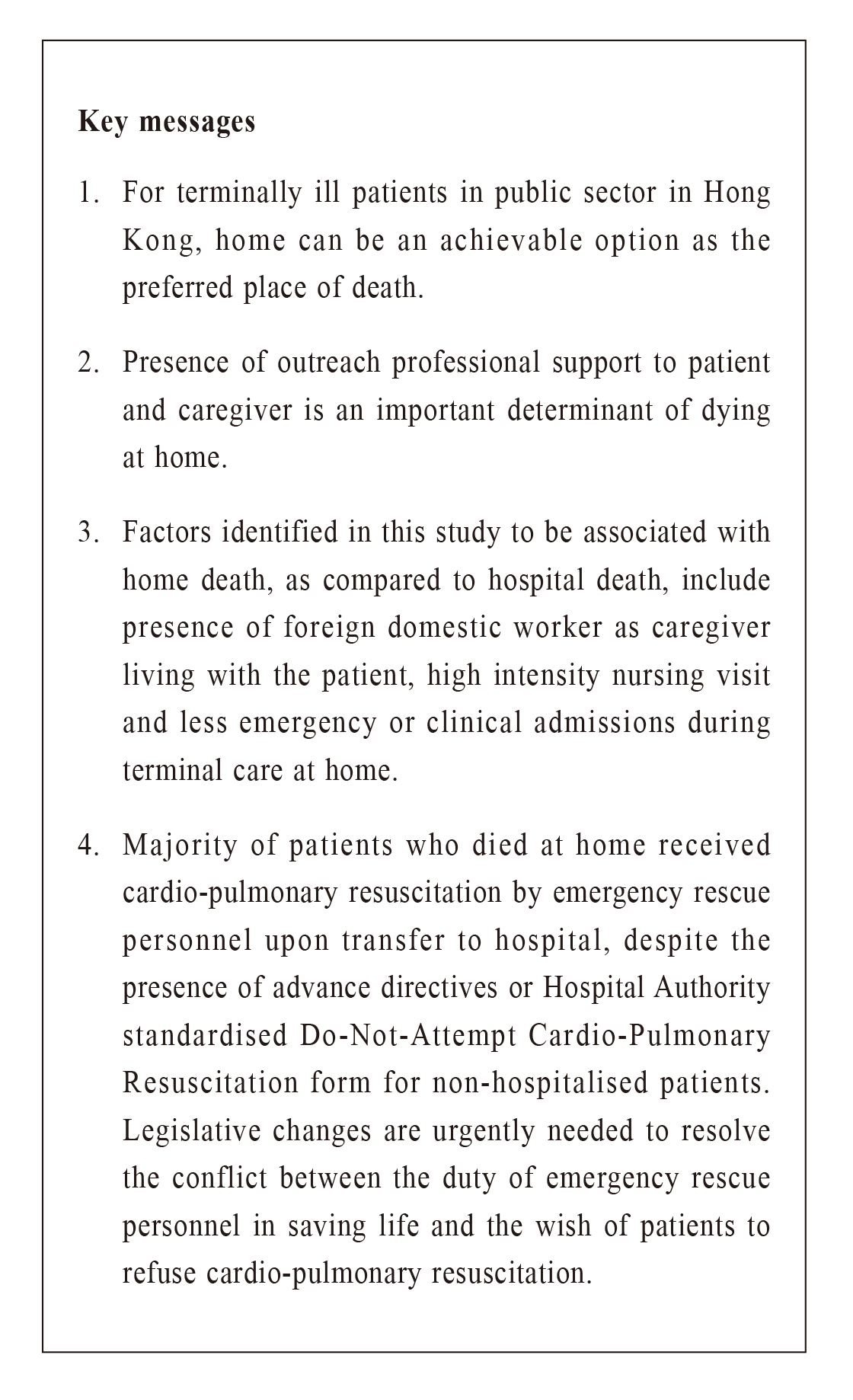
Despite the extremely low prevalence of home death
in HK, more than half of patients in this study died at
home. This suggested that home can be an achievable
option in Hong Kong as the preferred place of death.
Factors associated with place of death
The criteria for recruitment in the program are
known to be factors associated with an increased
likelihood of home death, including the preference
of patient18,19, caregiver18,24 and family19 for dying
at
home, as well as the presence of relatives18 or informal
caregiver19 living with the patient. The presence of
home palliative care provided by doctors and nurses is
another important factor associated with an increased
likelihood of home death18,19,24,25
When comparing patients dying at home and those
in hospital in this study, having FDH as caregiver living
with patients is found to be associated with home death.
FDHs comprised 5% of HK population and covered
11% of local households.26,27 As most of the patients
who died at home (81.3%) and in hospital (95.2%)
already have full-time family caregivers living with
them, the specific caregiving role shared by FDH would
worth further exploration. The employment of FDH
may also indirectly reflect a better social condition and
higher economic status which favour home death.18,28,29
The current study does not find other sociodemographic
or illness factors associated with place of death. Lower
psychological stress in caregivers has been reported to
be associated with home death, but our study does not
find significant difference in the stress by RSS between
family caregivers of patients dying at home and in
hospital (10.5 and 13, Mann-Whitney U = 79.0, n1 =
22, n2 = 17, p = 0.624). A reason may be that families
under obvious high psychological stress could have
been excluded from the programme by the clinical team
upon recruitment assessment.
In this study, more patients who died at home than
those in hospital received high intensity of nursing home visit (5 times or more per
week). It is consistent
with previous review that intensity of home care
increased odds of home death18, reflecting the crucial
and heightened role of community nursing support in
the last days of life for patients dying at home. Patients
who died at home had fewer emergency admissions
through AED, consistent with previous report that prior
crisis related re-hospitalization would predict hospital
death.24 Patients who died in hospital had more clinical
admissions to PC ward and appeared to have received
longer duration (median 109 versus 54 days, not
statistically significant) of PC service. The experience
of support from in-hospital PC team or hospice unit
may increase the acceptance of admission for symptom
relief and has been identified as a determinant of
hospital death.19
Around 40% of patients admitted to hospital
when they were imminently dying, despite initial
preference on home death and presence of both lay
and professional support at home. Evolving physical
symptoms, which might not be well anticipated by
patients and caregivers, were the major reason of
admission. As an example, shortness of breath was
known to have its prevalence increased significantly
before death and was a common reason for PC patients
to visit AED.30 Taking care of a dying family member
at home could be physically and psychologically very
demanding. We found that some patients’ family might
finally choose hospital death, especially when the
imminently dying patient became mentally dull and was
apparently not aware of his/her location.
Professional support in community for patients
and families in the last days of life
Whether a patient with advanced illness can die
at home depends heavily on the healthcare services
available in the community. This study captured the
holistic approach in the dying-at-home programme
which includes symptom management to maintain
comfort and dignity as well as communication and
shared decision with the dying patient and people
important to them.31 For patients in community,
evidence suggested that palliative home care services
increased odds of dying at home and were effective
in reducing symptom burden.32 The importance of
caregiver education and empowerment could not be
overemphasised since the sustainability of keeping
terminally ill patients at home depends on how able they
are to care for their loved ones at home.18 The fact that
caregivers in this programme were trained to monitor
fluid and medication infusion and were informed of
the dying process may both have contributed to home
death.24
Use of strong opioids via CSCI is not feasible in
the dying-at-home programme. It is due to the present
lack of corporate guidance which could back up the
administration of dangerous drug (DD) via syringe
driver outside hospital setting. CSCI is a common
technique in contemporary palliative care and the use of
the compact syringe driver for CSCI allowed symptom
control at home for patients who no longer tolerate
oral medication.33 Use of strong opioids via CSCI is an
important intervention for patient dying at home with
pain and/ or dyspnoea. Guidelines on use of syringe
driver with DD in community should be established by
HA to overcome this barrier in the public sector.
Legal and logistic issues of home death in
Hong Kong
Without the availability of ad hoc doctor visit
for certification of death in the dying-at-home
programme, all patients would be sent to AED just
after death. Unfortunately, majority (87.5%) of these
patients had received CPR delivered by ERP, despite
the presentation of the valid and applicable advance
directives made by the patients or the DNACPR
forms written by the doctors. Currently in HK, ERP
of Fire Services Department (FSD) are bound by Fire
Services Ordinance (FSO) to perform CPR and other
related resuscitation to any person who appears to
need prompt or immediate medical attention.34 This
issue was addressed by Food and Health Bureau
in a public consultation in 2019.35 The recently
released Consultation Report have proposed measures
including the use of a statutory DNACPR form and the
corresponding amendment in FSO provisions to accept
this form.36 Such legislative changes are urgently
needed to resolve the conflict between the wish of the
patient and the obligation of ERP.
Before the legal resolution, an alternative way
might come from partnership with family physicians, in
which a registered doctor who has attended the patient
during his/her last illness can certify the death at home
and issue the Certificate of the Cause of Death (Form
18).37 With Form 18, the family can proceed to register
the death and thence legally move the body37 from
home through funeral service
Limitations
This study has a small sample size but provided
the very low preference of dying at home in Hong
Kong, this study offered initial findings in this area of
local research. Patients recruited in the dying-at-home
program were highly selected: clear preference for dying
at home, presence of full-time caregiver and receiving
a high-intensity professional support in community.
Therefore, the findings may not be generalisable to
other people with advanced life-limiting illness in
Hong Kong. However, the recruited patients still cover
a wide range of cancer and non-cancer diagnoses, age
groups and social background which may still provide
meaningful account of the profile of this specific group
of patients.
Conclusion
The findings of this study suggest that home as a
preferred place of death is achievable in HK. Presence
of community palliative care service supporting patient
and caregiver is an important determinant. To avoid
unnecessary and futile CPR, there is a pressing need in
legislative changes to resolve the conflict between the
duty of ERP in saving life and the wish of patients to
refuse CPR.
Jeffrey SC Ng, MBBS, FHKAM (Medicine)
Associate consultant,
Department of Medicine, Haven of Hope Hospital, Hong Kong
Specialist in Family Medicine
Pui-chi Chiu, MSc, FHKAN (Palliative Care)
Advance Practice Nurse,
Department of Medicine, Haven of Hope Hospital, Hong Kong
Po-tin Lam, MBChB, FHKAM (Medicine)
Consultant,
Department of Medicine and Geriatrics, United Christian Hospital, Hong Kong
Ka-yee Lee, MNurs, FHKAN (Community and Public Health
Nursing)
Department Operations Manager,
Community Nursing Service, Kowloon East Cluster, Hong Kong
Kai-ming Li, MBBS, FHKAM (Emergency Medicine)
Consultant,
Accident and Emergency Department, United Christian Hospital, Hong Kong
Correspondence to: Dr. Jeffrey SC Ng, Department of Medicine,
Haven of Hope
Hospital, 8 Haven of Hope Road, Tseung Kwan O, Hong Kong SAR.
E-mail: ngscj@ha.org.hk
References:
-
Smith R. A good death. An important aim for health services and for us all.
BMJ. 2000;320(7228):129-130
-
De Roo ML, Miccinesi G, Onwuteaka-Philipsen BD, et al. Actual
and Preferred Place of Death of Home-Dwelling Patients in Four
European Countries: Making Sense of Quality Indicators. PLOS ONE.
2014;9(4):e93762.
-
Sadler E, Hales B, Henry B, et al. Factors Affecting Family Satisfaction with
Inpatient End-of-Life Care. PLOS One. 2014;9(11):e110860.
-
Gomes B, Calanzani N, Gysels M, et al. Heterogeneity and changes in
preferences for dying at home: a systematic review. BMC Palliat Care.
2013;12:17.
-
Tang ST. Meanings of dying at home for Chinese patients in Taiwan with
terminal cancer: a literature review. Cancer Nursing. 2000;23(5):367-370.
-
Hospital Authority. Strategic Service Framework for Palliative Care (issued
on 7 August 2017). Available at https://www.ha.org.hk/haho/ho/ap/PCSSF_1.
pdf. Accessed on 7 Dec 2020.
-
Chung RY, Wong EL, Kiang N, et al. Knowledge, Attitudes, and Preferences
of Advance Decisions, End-of-Life Care, and Place of Care and Death in
Hong Kong. A Population-Based Telephone Survey of 1067 Adults. J Am
Med Dir Assoc. 2017;18(4):367.e19-367.e27.
-
Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: a qualitative
systematic literature review of patient preferences. J Palliat Med.
2000;3(3):287-300
-
Hong TC, Yau LM, Ng CC, et al. Attitudes and expectations of patients with
advanced cancer towards community palliative care service in Hong Kong.
Proceedings of the 2010 Hospital Authority Convention; 2010 May 10-11;
Hong Kong.
-
Woo KW, Kwok OL, Ng KH, et al. The preferred place of care and death in
advanced cancer patients under palliative care services. Paper presented at
the 10th Hong Kong Palliative Care Symposium; 2013 Aug 10
-
Liu FCF, Lam C. Preparing cancer patients to die at home. Hong Kong
Nursing Journal. 2005;4(1), 7–14.
-
Luk JKH, Liu A, Ng WC, et al. End-of-life care in Hong Kong. Asian J
Gerontol Geriatr 2011;6:103–106
-
Gonçalves-Bradley DC, Iliffe S, Doll HA, et al. Early discharge hospital at
home. Cochrane Database Syst Rev. 2017;6(6):CD000356.
-
DLeung DY, Lee DT-F, Lee IF, et al. The effect of a virtual ward program
on emergency services utilization and quality of life in frail elderly patients
after discharge: a pilot study. Clinical Interventions in Aging. 2015;10:413-
420.
-
Cap. 504 Coroners Ordinance. Schedule 1 [ss. 2, 4 & 55]. Part 1 Reportable
Deaths. Available at https://www.elegislation.gov.hk/hk/cap504. Accessed on
7 Dec 2020.
-
Patient Safety & Risk Management Department / Quality & Safety Division,
Hospital Authority. Guidance for HA Clinicians on Advance Directives
in Adults (2020). Available at https://www.ha.org.hk/haho/ho/psrm/
ADguidelineEng.pdf. Accessed on 7 Dec 2020.
-
Patient Safety & Risk Management Department / Quality & Safety Division,
Hospital Authority. HA Guidelines on Do-Not-Attempt Cardiopulmonary
Resuscitation (DNACPR) (2020). Available at
https://www.ha.org.hk/haho/ho/psrm/DNACPRguidelineEng.pdf. Accessed on 7 Dec
2020.
-
Gomes B, Higginson IJ. Factors influencing death at home in terminally
ill patients with cancer: systematic review. BMJ. 2006;332(7540):515-521.
Erratum in: BMJ. 2006;332(7548):1012.
-
Costa V, Earle CC, Esplen MJ, et al. The determinants of home and nursing
home death: a systematic review and meta-analysis. BMC Palliative Care.
2016;15:8.
-
Anderson F, Downing GM, Hill J, et al. Palliative Performance Scale (PPS):
A New Tool. J Palliat Care 1996; 12(1):5-11.
-
Francis Lau, G. Michael Downing, Mary Lesperance, et al. Use of Palliative
Performance Scale in End-of-Life Prognostication. J Palliat Med 2006;
9(5):1066-1075.
-
Ulstein I, Bruun Wyller T, Engedal K. The relative stress scale, a useful
instrument to identify various aspects of carer burden in dementia? Int J
Geriatr Psychiatry.2007;22(1):61–67.
-
Ulstein I, Wyller TB, Engedal K. High score on the Relative Stress Scale,
a marker of possible psychiatric disorder in family carers of patients with
dementia. Int J Geriatr Psychiatry. 2007;22(3):195-202.
-
Fukui S, Fukui N, Kawagoe H. Predictors of place of death for Japanese
patients with advanced-stage malignant disease in home care settings: a
nationwide survey. Cancer. 2004;101(2):421-429.
-
Lee YS, Akhileswaran R, Ong EHM, et al. Clinical and Socio-Demographic
Predictors of Home Hospice Patients Dying at Home: A Retrospective
Analysis of Hospice Care Association's Database in Singapore. J Pain
Symptom Manage. 2017;53(6):1035-1041.
-
Immigration Department, HKSAR. Statistics on the number of foreign
domestic helpers in Hong Kong provides figures concerning the number of
foreign domestic helpers in Hong Kong https://data.gov.hk/en-data/dataset/
hk-immd-set4-statistics-fdh. Accessed on 7 Dec 2020.
-
Research Office, Legislative Council Secretariat, HKSAR. https://www.legco.
gov.hk/research-publications/english/1617rb04-foreign-domestic-helpers-and-evolving-care-duties-in-hong-kong-20170720-e.pdf.
Accessed on 7 Dec 2020.
-
Gatrell AC, Harman JC, Francis BJ, et al. Place of death: analysis of cancer
deaths in part of North West England. J Public Health Med. 2003;25(1):53-8.
-
Barclay JS, Kuchibhatla M, Tulsky JA, et al. Association of hospice
patients' income and care level with place of death. JAMA Intern Med.
2013;173(6):450-6.
-
Kamal AH, Maguire JM, Wheeler JL, et al. Dyspnea review for the
palliative care professional: treatment goals and therapeutic options. J Palliat
Med. 2012 Jan;15(1):106-14.
-
National Institute for Health and Care Excellence. Care of dying adults in
the last days of life. Published 2 March 2017. Available at https://www.nice.
org.uk/guidance/qs144. Accessed on 7 Dec 2020.
-
Gomes B, Calanzani N, Curiale V, et al. Effectiveness and cost-effectiveness
of home palliative care services for adults with advanced illness and their
caregivers. Cochrane Database of Systematic Reviews 2013, Issue 6. Art.
No.: CD007760.
-
Graham F, Clark D. The syringe driver and the subcutaneous route in
palliative care: the inventor, the history and the implications. J Pain
Symptom Manage. 2005;29(1):32-40.
-
Cap. 95 Fire Services Ordinance. Section 7 Duties of Fire Services
Department. Available at https://www.elegislation.gov.hk/hk/
cap95!en?pmc=1&m=1&pm=0. Accessed on 7 Dec 2020.
-
Food and Health Bureau. Public Consultation on End-of-life Care:
Legislative Proposals on Advance Directives and Dying in Place - Consultation
Document. Available at
https://www.fhb.gov.hk/download/press_and_publications/consultation/190900_eolcare/e_EOL_care_legisiative_proposals.pdf.
Accessed on 7 Dec 2020.
-
Food and Health Bureau. Legislative Proposals on Advance Directives and
Dying in Place – Consultation Report. Available at https://www.fhb.gov.
hk/download/press_and_publications/consultation/190900_eolcare/e_EOL_
consultation_report.pdf. Accessed on 7 Dec 2020.
-
Cap. 174 Births and Deaths Registration Ordinance. Part I Medical
Certificate of the Cause of Death. Available at https://www.elegislation.gov.
hk/hk/cap174?SEARCH_WITHIN_CAP_TXT=Certificate%20of%20the%20
Cause. Accessed on 7 Dec 2020.
|