
|
December 2021,Volume 43, No.4
|
Case Report
|
A case of continuous severe abdominal pain - Advice from The Medical Protection SocietyHeidi Mounsey HK Pract 2021;43:124-126 SummaryA patient had ongoing severe abdominal pain and was eventually diagnosed with a small bowel tumour; however, a claim was made that the diagnosis was delayed. The Medical Protection Society team assisted in this case. 摘要一位患有持續嚴重腹痛的病人,經過多次求診,最終診斷為小腸腫瘤。病人就對於診斷的延誤作出賠償的要求。Medical Protection Society 團隊協助會員跟進這個個案。 The caseMrs K, a 42-year-old insurance clerk complained of abdominal pain. She had had a history of dysmenorrhea and had been on the combined oral contraceptive pill. HistoryMonth, no. 1Mrs K contacted her GP practice on the telephone and spoke to Dr A to say that she had had on - going severe abdominal pain the evening before, and experienced heavy menstrual bleeding with clots that morning despite her having been on the oral contraceptive pill (OCP). The pain had now settled. Dr A suggested a trial of tranexamic acid to take as needed whenever Mrs K’s periods were heavy. Dr A advised her to book an appointment for a pelvic examination. Month, no. 2Mrs K attended the surgery for a face-to-face appointment four weeks after the telephone consultation, complaining of on-going heavy periods and abdominal pain; and she was examined and her complaints were reviewed by Dr B. Pelvic examination was found to be difficult due to Mrs K’s obesity and the heavy bleeding. Dr B referred her for a pelvic ultrasound scan as well as requested a range of blood tests, including a full blood count and the CA125 blood test. The ultrasound scan took place two weeks later and revealed two large fibroids. A referral to a gynaecologist was recommended by the ultrasonographer providing the scan report. The blood tests revealed Mrs K to be slightly anaemic which was attributed to the heavy menstrual bleeding. Over the telephone, Dr A discussed the results with Mrs K and established that Mrs K was experiencing bloating of her stomach after eating with intermittent abdominal pain, and that she wished to be referred to gynaecology for consideration of surgery. A referral to gynaecology was duly made. Month, no. 3The following few weeks passed by, and Mrs K contacted the surgery again when a telephone consultation with Dr A took place, during which she described an episode of severe abdominal pain throughout the night some days earlier that had then settled. The pain was considered to be due to the fibroids and mefenamic acid was prescribed for her to take whenever needed. Month, no. 4Mrs K underwent a further telephone consultation with Dr A, complaining of ongoing abdominal bloating and three episodes of vomiting on the previous day. It was noted that Mrs K felt a tendency of wanting to vomiting whenever her period was due. She was prescribed codeine and paracetamol as she complained mefenamic acid to be ineffective. Her gynaecology appointment was noted to be due in another two weeks’ time, by which time Mrs K would have been suffering her symptoms for over four months! Month, no. 5The gynaecology team reviewed Mrs K and repeated another pelvic ultrasound. Due to the views were not very clear, the team requested an MRI scan for better imaging of the fibroids. This time the MRI scan revealed a very large fibroid and Mrs K was advised for laparoscopic hysterectomy, although she was at the same time also told she needed to lose weight before this could take place. Month, no. 6 to 11Over the next few months, Mrs K continued to present herself to the GP practice complaining of spasmodic upper abdominal pain, vomiting and bloating. A diagnosis of biliary colic was considered and she was referred initially for an ultrasound scan to assess for the presence of gallstones, and then to the gastroenterology team. Although the ultrasound scan did not demonstrate gallstones, both the gastroenterology team and the GPs continued to consider biliary colic being the most likely cause for her on-going and intermittent symptoms. Month, no. 12Mrs K was ultimately admitted to hospital as an emergency for severe abdominal pain and a raised temperature, suspected to be caused by ascending cholangitis. However, subsequent investigations revealed a small bowel stricture which led to her undergoing an emergency laparotomy and small bowel resection. Histology demonstrated a small bowel adenocarcinoma. She was advised to undergo adjuvant chemotherapy. Mrs K subsequently brought a claim against Dr A, alleging that she was experiencing severe pain at the time of the initial telephone consultation and should have been advised to attend the practice the same day for a face-to-face appointment. Mrs K also alleged that subsequent to her reporting an episode of severe abdominal pain that had lasted throughout the night, Dr A should have arranged a face-to-face same day appointment for examination and reviewed; and again, at the time Mrs K reported vomiting. It was alleged that had she been reviewed in-person on these occasions, she would have been referred to secondary care earlier and the tumour would have been identified at an earlier time-point, therefore avoiding several months of unpleasant symptoms and allowing surgery to be performed as an elective case. Further allegations were also made against the other clinicians who had reviewed Mrs K during this time. Final outcomeThe case was assisted by Medical Protection Society’s medical and legal team, and Dr A was considered to have acted appropriately. The team also felt that it was unlikely that, even had Mrs K been seen face-to-face on any of the occasions, or that she was referred sooner to secondary care, the tumour would have been identified significantly earlier. A GP expert was also instructed to give his opinion. The expert was clear that, on the basis of the medical records and Dr A’s comments, it was not mandatory for a doctor to offer a face-to-face appointment the same day at any of her telephone consultations. The expert did, however, comment that had symptoms been ongoing at the time of the consultations, then Dr A should try to have established the severity of the pain or vomiting and would likely offer a same day appointment for review and examination. On receipt of the experts’ reports, the case was again fully reviewed by Medical Protection Society’s medical and legal team, and it was agreed that a letter of response, defending the actions of Dr A, should be drafted, and that the offer by Mrs K’s solicitors of early settlement should be rejected. Following receipt of the Medical Protection Society’s letter of response, Mrs K’s solicitors discontinued the claim against Dr A. In this case, the clear and extensive documentation made by Dr A, enabled the defence of Dr A’s decision not to invite the patient for face-to-face review at the time of the various telephone consultations. 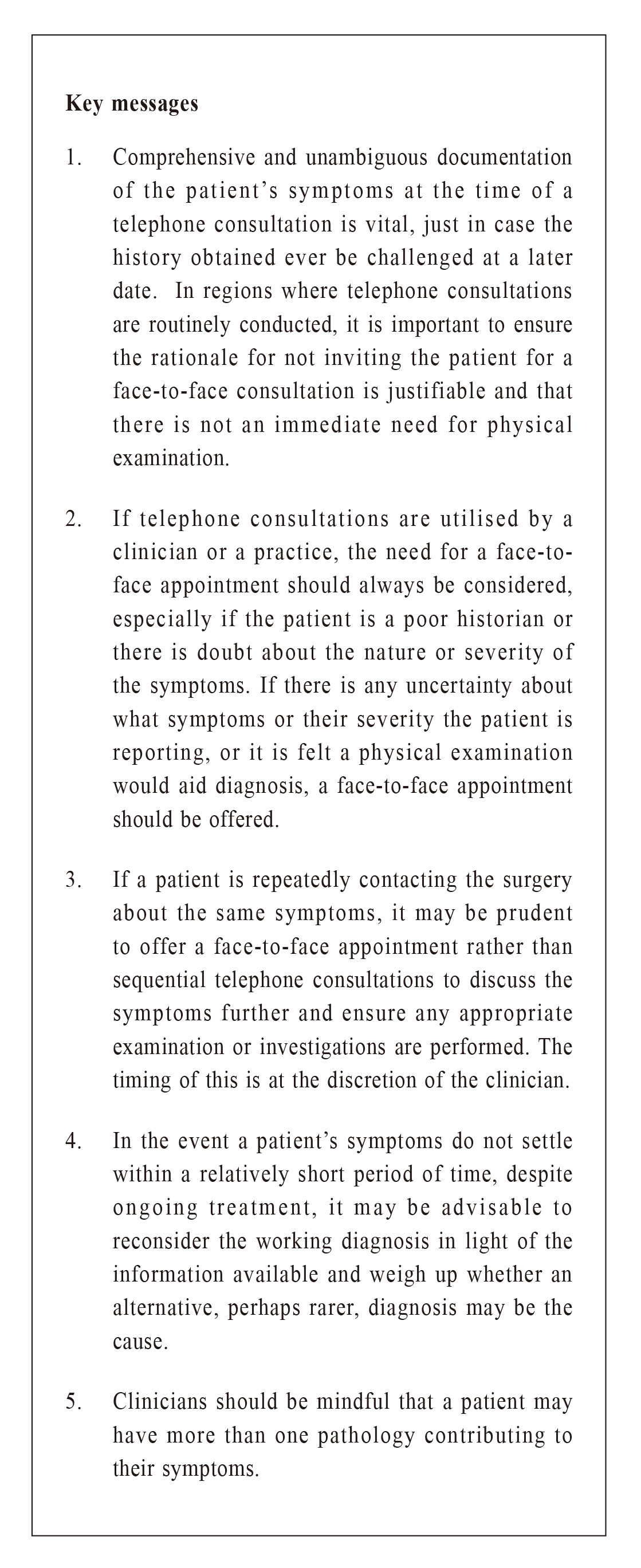
Heidi Mounsey, BMBS (Nottingham), FRCA (Royal College of Anaesthetists)
Correspondence to: Dr Heidi Mounsey, Medical Protection Society, Victoria House,
2 Victoria Place, Leeds LS11 5AE, United Kingdom.
References:
|
|