
|
Jun 2020,Volume 42, No.2
|
Update Article
|
Menopause management – update on hormone replacement therapyPui-yi Siu 蕭珮儀,David VK Chao 周偉強 HK Pract 2020;42:30-35 SummaryMenopause is associated with a variety of short term symptoms and long term health consequences. Hormone therapy remains the most effective treatment for vasomotor symptoms and the genitourinary syndrome of menopause. The risks of hormone therapy depend on factors such as type and dose of hormone, timing of initiation and duration of therapy. Decision on treatment should be individualised, with periodic evaluation of benefits and risks of continuing or terminating hormone therapy. 摘要更年期與一系列的短期症狀和長期健康後果有關。荷爾蒙療 法仍然是治療血管舒縮症狀和更年期泌尿生殖系統綜合症的 最有效方法。荷爾蒙治療的風險取決於多種因素,例如激素 的類型和劑量,開始使用的年齡和治療的持續時間。治療的 決定應因人而異,須定期評估繼續或終止荷爾蒙治療的益處 和風險。 IntroductionMenopause is an important stage of a woman’s life cycle; it signifies the end of menstruation and reproduction. Menopause may also be accompanied by vasomotor and genitourinary symptoms which maybe due to a decrease in the oestrogen hormone levels. Although hormone therapy is the most effective treatment for menopausal symptoms, studies have shown there are conflicting views about benefits and risks. As family physicians, we are in a good position to offer evidence-based information and help women make informed decisions about the management of their menopause. This article aims to provide updated information on hormone therapy for menopausal women. The consultation for menopausal symptomsMedical history and examinationMenopause is defined as the stage of a woman’s life after a 12 months’ period of amenorrhoea. The average age of menopause among Hong Kong women is 51. During transition to menopause, women may have a variety of symptoms due to fluctuating ovarian function and hormone levels. 1 The most common conditions that might present to the primary care providers are troublesome vasomotor symptoms, mood changes and osteoporosis. Comprehensive assessment is necessary to determine the most suitable management plan . During the consultation, history should not only include symptoms and the impact on the patient’s quality of life, the type of menopause (natural or iatrogenic) or premature ovarian failure as well as need for contraceptive practices. Personal or family history of breast, ovarian and endometrial cancer; venous thromboembolism, migraine, osteoporosis, cardiovascular risk factors, heart disease and stroke should be documented. Physical examination for weight, height and blood pressure should be performed. 2 Lifestyle adviceThe consultation provides an opportunity to have a discussion on healthy lifestyles. Weight gain at midlife in women is due to aging rather than menopause. But hormonal changes during the transition to menopause could lead to increase in abdominal fat and decline in lean body mass. Women should be encouraged to adopt a healthy balanced diet and regularly exercise to prevent weight gain and preserve muscle mass. 2 In addition,smoking cessation and minimising alcohol intake are also important for general health and wellbeing. 3 Screening for cancer, for osteoporosis and for cardiovascular riskThe consultation is also a good time to discuss screening for diseases which would be encountered in later life. Women should be encouraged to participate in local screening programmes for cervical and colon cancers. 4 At this point of time, there is insufficient evidence for or against population-based mammography screening for asymptomatic women at average risk in Hong Kong. Women should be advised to be breast aware (be familiar with the normal look and feel of their breasts) and consult doctors promptly if suspicious symptoms appear. Individuals considering breast cancer screening should be adequately informed about the benefits and harms. 5 Patients at risk of osteoporotic fracture can be identified opportunistically by using Fracture Risk Assessment Tool (FRAX). 2 FRAX can be accessed online (https://www.sheffield.ac.uk/FRAX/index.aspx) to calculate the 10-year probability of fracture. It can be used for people aged between 40 and 90 years, either with or without bone mineral density. Assessment for cardiovascular risk would also be advisable. 2 Diagnosis of menopauseThe diagnosis of menopause could be made without laboratory tests in otherwise healthy women aged over 45 years whose monthly periods maybe irregular or absent with menopausal symptoms. FSH can be considered for younger women with suspected premature ovarian failure. 2,3 Hormone therapy - Indications and contraindicationsPharmacological management of menopausal symptomsis classified into hormonal or non- hormonal. In recent years, it has become common to use the term Hormone Therapy (HT) instead of Hormone Replacement Therapy (HRT) because there is a controversy that the use of hormones in this context is not strictly ‘replacement’. However, the two terms, menopausal HT (MHT) and HRT can be used interchangeably. 6 HRT is used in this article since it is the more commonly used term in Hong Kong. HRT is approved by U.S. Food and Drug Administration (FDA) for four indications: bothersome vasomotor symptoms; prevention of bone loss; hypoestrogenism (caused by hypogonadism, premature ovarian insufficiency and surgical menopause) and genitourinary symptoms. 7 Contraindications to the use of HRT are personal history of breast or endometrial cancer, unexplained vaginal bleeding, venous thrombosis, acute liver disease and established cardiovascular disease. 1,2,6,7The presence of cardiovascular risk factors is not a contraindication to HRT if they are optimally managed. 1,3One more thing, it should be noted with HRT that endometriosis, if present, may be reactivated, migraine headaches might be worsen and uterine fibroid may become even larger. 7 Management of short term menopausal symptoms using HRTVasomotor symptomsVasomotor symptoms may becaused by thermoregulatory dysfunction, which begin during perimenopause and may last for as long as 7.4 years or even more. 7 Although some Chinese women suffer from severe vasomotor symptoms, their problems tend to be less severe than Caucasians. 6 HRT with systemic oestrogen is the most effective treatment for vasomotor symptoms. The risk-benefit profile is more favourable for symptomatic women starting HRT before the age of 60 years or within the 10 years after menopause. 1,2,3,7 Genitourinary syndrome of menopause (GSM)GSM is the collection of symptoms and signs as a result of post-menopausal oestrogen deficiency. Changes occur in the labia, vagina, urethra and bladder, leading to genital symptoms of dryness, burning and irritation; sexual symptoms of lack of lubrication and pain; and urinary symptoms of urgency, dysuria and recurrent urinary tract infections. 2,7 Topical vaginal oestrogen therapy is useful for vaginal and sexual symptoms, as well as prevention of recurrent urinary tract infections, overactive bladder and urge incontinence. Psychological symptomsHRT could be considered to relieve low mood that emerges as a result of menopause. 3 HRT in the form of low-dose oestrogen or progestogen have been noted to alleviate chronic insomnia in menopausal women. 7 Long term benefits and risks of HRTSince the publication of Women’s Health Initiative (WHI) in 2002, many clinicians and the general public perceived HRT as an unsafe treatment. The WHI trial reported HRT was associated with increased risks of breast cancer, cardiovascular disease and venous thromboembolism. 8 Use of HRT had declined in a sustained fashion across a variety of patient subgroups since then. 9 Subsequent re-analyses of the WHI data, as well as other randomised trials and observational studies, have led to a change in the understanding of the benefits and risks of HRT. International menopause organisations now advise that the reports of harm attributed to HRT were overestimated. 1 WHI was criticised for its recruiting bias, with limited enrollment of women with bothersome vasomotor symptoms who were aged under 60 years or fewer than 10 years from onset of menopause – the group of women for whom HRT is primarily indicated. 7 OsteoporosisStandard-dose HRT prevents bone loss in post menopausal women by in hibiting osteoclast-driven bone resorption and reducing rate of bone remodeling. HRT is effective in the prevention of hip and vertebral fractures. 6,7 In the WHI trial, HRT had significantly reduced incidence of hip fracture by 33%, with overall 6 fewer fractures per 10,000 person-years. 7 For women younger than 60 years or who are within the first 10 years of menopause, HRT is effective and appropriate for the management of vasomotor symptoms and prevention of osteoporosis-related fractures in the absence of contraindications. 10 Women should be informed that the benefit of bone protection decreases once treatment stops, but no rebound in fracture risk has been found. 3,7 Coronary heart disease (CHD)HRT does not increase the risk of CHD when initiated in healthy postmenopausal women who are under 60 years of age, or who are within their first 10 years of menopause. 1,3,7 Randomised control trials (RCT), observational data and meta-analyses provide evidence that standard-dose oestrogen-alone HRT may decrease CHD and all-cause mortality in this group of younger women. 3,10 However, if HRT is initiated after more than 10 years from the onset of menopause, and more definitely, if 20 years, there is an increased risk of CHD. 7 StrokeData concerning HRT and risk of stroke is controversial. For women younger than 60 years or who were within 10 years of menopause, a meta-analysis of RCTs showed no increased risk of stroke; while a subgroup analyses of WHI studies found a rare but absolute risk of stroke. For older women, initiation of HRT was associated with increased risk of stroke. 7 Women should be informed that the baseline risk of coronary heart disease and stroke for perimenopausal women varies from one to another according to the individual’s own cardiovascular risk factors. 3 HRT is not indicated for primary or secondary cardioprotection. 7 Established cardiovascular disease is a contraindication for HRT. 6 Nevertheless, the presence of cardiovascular risk factors is not a contraindication as long as the cardiovascular risks are well controlled. 3 Venous thrombo-embolism (VTE)The risk of VTE is increased with oral HRT. 1,3,7 The use of transdermal HRT has not been associated with increased VTE risk and should be considered for menopausal women who are at an increased risk of VTE, such as those with BMI over 30kg/m2. 1,3 Breast cancerLast but not the least, breast cancer is often the main concern for women and clinicians. The effect of HRT on breast cancer risk may depend on the type of HRT, dose, duration of use, route of administration, prior exposure, and individual characteristics. 7 In the WHI study, there was a rare but absolute risk of breast cancer (<1 additional case/1,000 person-years of use) with the daily continuous-combined oestrogen and progesterone arm; while there was an insignificant risk reduction in the oestrogen alone arm. 6,7 A new meta-analysis published in Lancet 2019 has shown that the total risk of breast cancer associated with HRT is higher than previously estimated. Every HRT type, except vaginal oestrogen, is associated with excess breast cancer risks. The risks are greater for oestrogen-progestogen than oestrogen only preparations. There is little or no increase in risk with current or previous use of HRT for less than 1 year; but there is an increased risk with HRT use for more than 1 year, increasing further with longer duration of HRT use. Risk of breast cancer is lower after stopping HRT than current user, but remains increased in ex-HRT users for more than 10 years compared with those who never used HRT. For women who use HRT for similar durations, the total number of HRT-related breast cancers by age 69 years is similar whether HRT is started in her 40s or in her 50s. 11,12 This new study only provided information of an increased incidence of breast cancer with HRT, but did not address mortality. Hence findings must be weighed against a recent systematic review which showed that star ting HRT close to menopause may reduce all-cause mortality. The overall benefit and risk ratio in using HRT for treating menopausal symptoms should be individualised for each patient. Women should be counselled that other factors like body weight and alcohol consumption also pose significant risks to breast cancer. 13 To facilitate communication with patients, clinicians can present the risk in terms of figures during consultation. (Table 1) 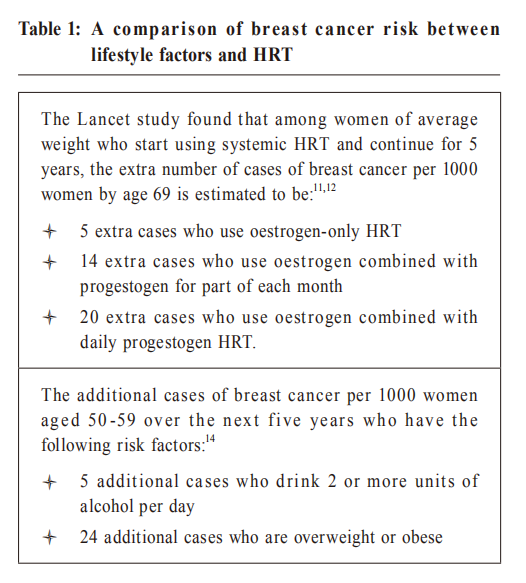
Prescription of HRTType – cyclical and continuousHRT consists of continuous oestrogen for symptom management and other physiological effects, with an addition of progestogen for endometrial protection for women with intact uterus. 1 Progestogen can be given either cyclically or continuously. Combined cyclical HRT usually results in regular withdrawal bleeding at the end of each progestogen cycle. 6 For women who had their last menstrual period less than 1 year, combined cyclical HRT is recommended because continuous combined HRT may cause irregular bleeding in these women. 1,6Depending on the patient’s preference, this can be changed to continuous combined HRT after 12 months. 1 For women with an established menopause (more than 12 months), continuous combined HRT can be given to help women remain amenorrhoeic. Route of administrationOral and transdermal HRT options are available. The choice is determined on the basis of known side effect profiles, individual woman’s health risks and personal preferences. 1,7Transdermal therapy can be considered for women with gut disorder affecting oral absorption, previous or family history of VTE, obesity, inadequate blood pressure control, migraine, current use of medication that induces hepatic enzymes and gall bladder disease. 15 Topical vaginal oestrogen (e.g. cream or pessary) is preferred over systemic therapies if the main concern is genitourinary syndrome of menopause (GSM). For those who are taking systemic therapies for vasomotor symptoms but GSM is not well controlled, additional topical oestrogen can be prescribed. 1 Dose – initiation and titrationHRT should be started at the lowest dose (estradiol 0.5mg or conjugated oestrogen 0.3mg) to reduce side effects and possible risks. 6,11,15 A follow up visit should be arranged within 3 months to assess effectiveness and adverse reactions to medication. 1,3 The dosage can be gradually increased if symptom control is inadequate. If bothersome side effects like fluid retention, breast tenderness or headache occur, dosage can be reduced accordingly.  Management of irregular bleeding on HRT Unscheduled vaginal bleeding is a common side effect of HRT within the initial 3 months of treatment. 3 For women using combined cyclical HRT, bleeding should occur around the time of progestogen withdrawal. But some women will be amenorrhoeic. If bleeding occurs at times other than this or is persistently irregular, endometrial biopsy is recommended. For women using continuous combined HRT, amenorrhoea should be achieved within about 4 months of starting treatment. Endometrial biopsy should be considered if bleeding occurs after spells of amenorrhoea. 6,15 Duration of treatmentOnce the appropriate HRT regimen is established, follow-up should be arranged at least annually to review regimen, assess efficacy and side effects of therapy; discuss any bleeding pattern; as well as evaluate risks and benefits of continuing therapy. 1,3,15 There is no arbitrary limit regarding the duration of use of HRT. 1,6,7,16 Decisions about continuation of HRT require individualisation, besides ongoing benefits and risks, personal preferences should also be considered. 7,16 Data from the WHI trial and other studies support safe use for at least 5 years in healthy women initiating treatment before age 60. 16Clinical judgment about extended use of HRT remain challenging since long-term follow-up data are complicated. Benefits include relief of persistent vasomotor symptoms, prevention of osteoporosis and treatment of GSM. For women younger than 60 years or within the first 10 years of menopause, HRT can reduce the risk of heart disease and all-cause mortality. 1,7On the other hand, risk of breast cancer increases as the duration of HRT use increases. 11,12 For patient swith GSM using local vaginal oestrogen, symptoms often come back when treatment is stopped. Systemic risks have not been identified with low dose local oestrogens. 3,16 However, long-term administration of unopposed vaginal oestrogen, with respect to the endometrium, lacks sufficient evidence to confirm its safety. 1 Patients should report unscheduled vaginal bleeding promptly to their health care providers. 3 If decision is made to discontinue HRT, it can be gradually reduced or stopped immediately. Step-wise reduction of HRT may reduce recurrence of symptoms in short term, but makes no differences to the symptoms in the longer term. 3 ConclusionMenopause may cause significant vasomotor and urogenital symptoms. HRT remains the most effective treatment and can be offered to symptomatic women. The risk-to-benefit ratio is lower for women during peri-menopause compared to those for older women. The decision for HRT should be individualised and tailored according to symptoms, past medical and family history, as well as individual preferences and concerns. Women currently live longer, primary care providers can empower women to make the best choices for their health and quality of life by providing them with a balanced information and supporting them in their decision making.
Pui-yi Siu, MBBS (HK), FHKCFP, FRACGP, FHKAM (Family Medicine)
David VK Chao, MBBS (HK), FHKCFP, FRACGP, FHKAM (Family Medicine)
Correspondence to:Dr Pui-yi Siu, Department of Family Medicine and
Primary
Health Care, United Christian Hospital, Kwun Tong, Hong Kong
SAR.
References:
|
|