
|
June 2019, Volume 41, No. 2
|
Discussion Paper
|
Palliative care in Hong Kong – past, present and futureWai-man Lam HK Pract 2019;41:39-46 SummaryPalliative care service first started in Hong Kong in 1982. Since then, in Hong Kong, it has developed into a territory wide service, largely specialist-led and hospital-based, and serving cancer and non-cancer patients. The lack of a territory wide cross-sector palliative care strategy, limited public awareness and community involvement in palliative care, and inadequate training in palliative care of healthcare professionals outside specialist palliative care settings, however, have resulted in not all patients in need being able to receive appropriate palliative care. It is time to review and revise the current approach to palliative care provision in Hong Kong. Collaboration between palliative care specialists and other healthcare professionals including primary care physicians is one of the keys for improvement. 摘要香港紓緩治療服務自一九八二年開展,以回應晚期癌症病人的需要,改善其生活質素。現在紓緩治療服務已覆蓋全港,主要由公營醫院的專科團隊為癌症和非癌症病人提供服務。但由於沒有一套全港性跨界別的紓緩治療服務發展策略、公眾的認知和參與不足、且其他醫療人員缺乏對紓緩治療的訓練,以致未能為所有有需要的病人提供適切的紓緩治療。現在該是檢視香港紓緩治療服務的時候了。紓緩治療專科團隊與其他醫療人員(包括基層醫療服務人員)的協作實為重要一環。 IntroductionThis article outlines the history of the development of palliative care service in Hong Kong. The service gaps, strengths and weaknesses, opportunities and threats, and barriers to its development will be discussed. Territory-wide palliative care strategy, generalist-specialist collaboration, and community engagement are called for. DefinitionThe World Health Organization defines palliative care as an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual. Palliative care:
Origin of the Modern Hospice MovementThe development of palliative care originated from a response to meet the needs and suffering of patients facing end of life from terminal illness and their family members caring for them. With the advances in modern medicine since the first half of 20th century, the focus of medical service and medical education has shifted to predominantly bringing cure, and the needs of dying patients were often not adequately met in modern medical system. Pain control was inadequate, symptoms were often left uneased, fears were not answered, and spiritual needs were often unrecognized. In response to the unmet needs, the modern hospice movement flourished in the western world in the 1960s to 1970s, inspired by the pioneering work of St Christopher Hospice established in London in 1967 by Cicely Saunders. In 1974, Dr. Balfour Mount, the father of palliative care in Canada, coined the term palliative care to avoid the negative connotations of the word hospice in French culture. Now palliative care has taken root in most parts of the world, and is considered a basic human right. Early Development in Hong KongThe first palliative care service in Hong Kong was pioneered in Our Lady of Maryknoll Hospital in 1982. In the latter half of the 1980s, palliative care services were started in four other hospitals; namely Ruttonjee Hospital, Nam Long Hospital, Haven of Hope Hospital and United Christian Hospital, in response to the needs of the suffering terminally ill patients, predominantly cancer patients. With the support of the Society for Promotion of Hospice Care, a non-government organization founded in 1985, the first palliative home care team and the first stand-alone hospice, Bradbury Hospice, were established in 1988 and 1992 respectively. These early development initiatives helped in building up palliative care values and philosophies, skills and knowledge of palliative care teams, and early referral mechanisms. (Figure 1) Centrally-coordinated comprehensive palliative care serviceA major milestone of palliative care service development occurred in 1994 when palliative care became centrally funded and coordinated by the government under the auspices of the Hospital Authority. The impetus of this move was from the policy address of the Governor then who pledged that more patients would be able to live out their terminal illnesses in comfort and dignity. A comprehensive range of services was developed in designated palliative care units, including in-patient care, outpatient care, home care, consultative service, day care and bereavement care. The characteristics of the service organization included cluster-based arrangement, comprehensive service provision, multidisciplinary team approach, specialist-led service, and evidence-based practices via standards, guidelines and audits. The training of palliative care specialists was further consolidated by recognition of Palliative Medicine as a subspecialty under the Hong Kong College of Physicians in 1998.2 In 2002, Palliative Medicine was also established as a subspecialty under Clinical Oncology.3 Hence in Hong Kong there are palliative care specialists under internal medicine stream and clinical oncology stream. There is constant collaboration between physicians and oncologists in professional development, service organization, and clinical governance of palliative care in Hong Kong. During this period, palliative care has become part of the public health care system. Territory wide audits of various palliative care outcomes were performed. The post-graduate training course for palliative care nursing was also established. 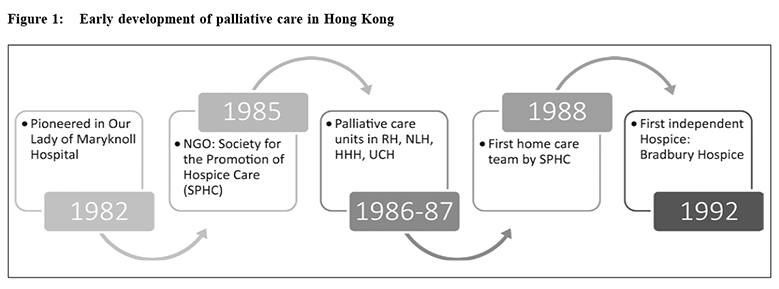
The number of palliative care services had grown to ten in 2004 and seventeen currently. (Figure 2) ResearchPalliative care research: towards an understanding of needsPalliative care workers and academia in Hong Kong endeavored to advance the knowledge and evidence base of palliative medicine by conducting research into various aspects of care. The McGill Quality of Life questionnaire was validated in Hong Kong Chinese4 and the Quality-of-Life Concerns in the End-of-Life questionnaire was locally developed.5 These quality-of-life assessment tools had been used in clinical care as well as palliative care research. Symptom distress for advanced cancer patients in the last week of life was studied which showed that fatigue, cachexia and anorexia were the most prevalent, but caregivers and physicians failed to rate them in agreement with patients.6 The spiritual aspects of palliative care had also been researched. In a qualitative study of spirituality among Hong Kong Chinese terminally ill patients, participants described spirituality as a unique personal belief that gives strength and relates to meaning of life, and they found quality interpersonal care from nurses to them giving them strength and supporting them spiritually.7 A study on hope in advanced cancer patients showed that hope experienced in this group of patients consisted of five components: living a normal life, social support, actively letting go of control, reconciliation between life and death, and wellbeing of significant others.8 Understanding patients’ spiritual needs is the first step to enhance their spiritual wellbeing by appropriate care. The caregivers’ needs and distress also came under the mandate of palliative care. An exploratory study on informal caregivers found that nearly all informal caregivers of patients with terminal cancer faced difficulties in rendering care in four main areas: relationship with the patients, emotional reactions to caring, physical demand, and restricted social life. Support from palliative home care nurses in skill training, information support and emotional support were found to be helpful.9 Another study on the family’s experience in caring for terminally ill cancer patients found that commitment was a precondition of the caregiving process and despite personal hardship, participants found the caregiving process meaningful to the patients and to themselves.10 The Modified Caregiver Strain Index had been validated among Hong Kong Chinese caregivers to aid the assessment and support of caregivers.11 The above are some examples of local palliative care researches that aim to understand more deeply the needs of patients and caregivers to enhance the care provided. 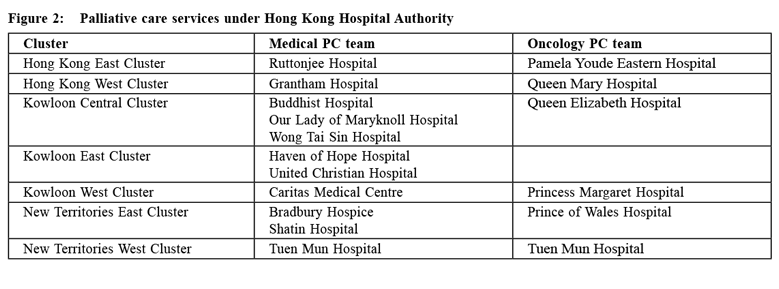
A systematic review in 2015 about end-of-life care research in Hong Kong identified 107 publications published in peer-reviewed journals between 1991 and 2014 and the research themes were diverse, including attitudes to or perceptions of death and dying, utilisation of healthcare services, physical symptoms or medical problems, death anxiety or mental health issues, quality of life, advance directive or advance care planning, supportive care needs, decision making, spirituality, cost-effectiveness or utility studies, care professionals’ education and training, informal caregivers’ perceptions and experience, and scale development or validation.12 The impact of palliative care service and the service gapsA retrospective study of 494 cancer patients who died in four public hospitals in Hong Kong showed that patients who had received palliative care had fewer acute admissions, shorter stay in acute wards, fewer admissions to intensive care setting, fewer invasive interventions initiated in the dying phase, larger number of symptoms addressed, higher likelihood of receiving medications for symptom control, more Do-Not-Resuscitate orders in place, and fewer cardiopulmonary resuscitations performed compared to those who had not received palliative care. These findings reflected that palliative care service had made a positive impact on end-of-life care.13 A pre- and post-test evaluation of a palliative care programme, comprising symptom management, intensive communication on advance care planning and psychosocial interventions, for patients suffering from life-limiting diseases demonstrated a positive effect on quality of life, improved understanding and active participation in advance care planning, reduction in hospital readmissions and shorter hospital stays.14 Moreover, a retrospective review comparing non-cancer and cancer deaths revealed the service needs of patients dying of non-cancer diseases, including chronic renal failure, chronic obstructive pulmonary disease and congestive heart failure. Only 1.4% of deceased non-cancer patients had received palliative care as compared to 79.2% of cancer patients. In their dying phase, non-cancer patients had more intensive utilisation of public health care, more invasive interventions initiated, fewer symptoms documented, less analgesics and sedatives prescribed, fewer Do-Not-Resuscitate orders in place, and more cardiopulmonary resuscitations performed.15 A study of symptom burden and quality of life in end stage renal disease showed that both patients on dialysis and those under palliative care service had comparable symptom prevalence and intensity, significant symptom burden and impaired quality of life.16 The palliative care needs of residents in Homes for the Elderly are also often inadequately met. A study on the needs of elderly advanced cancer patients in homes for the elderly showed that more than 60% suffered from physical and/or psychological symptoms and 22.4% had poor to fair symptom control17, but a study of care staff in these care homes revealed a lack of understanding about palliative care.18 These studies pointed out the service gaps in patients with non-cancer diseases and residents in homes for the elderly. In response to the service needs, palliative care service for non-cancer patients was developed and coordinated under Hospital Authority in 2010 to provide comprehensive palliative care to patients suffering from end stage renal diseases, chronic obstructive pulmonary disease, advanced heart failure, and neurological disorders. Since 2015, the End-of-Life Care Program in Residential Care Homes for the Elderly (RCHE) was gradually implemented to provide more coordinated and appropriate care to terminally ill residents in RCHEs through advance care planning, on-site support, direct clinical admission, psychosocial and spiritual support, and training and empowerment of staff in RCHEs.19 Recent DevelopmentsPalliative care: Setting the scene for the future (2008)In 2008, the Position Paper of the Hong Kong College of Physicians in 2008 titled “Palliative Care: Setting the Scene for the Future” was published. It pointed out the gap between the existing palliative care service provision in Hong Kong which was then characterised by specialist led services, largely hospital-based care, and higher focus on cancer patients and the anticipated escalating needs for palliative care due to the ageing population, rising prevalence of patients suffering from chronic debilitating diseases, high number of patients dying in non-palliative care acute settings, and inadequate palliative care development in private sector and in the community. The Position Paper called for some initiatives for further advancement of palliative medicine including timely review of palliative medicine and its interface with other medical subspecialties, promotion of palliative care for non-cancer patients, earlier initiation of palliative care in the disease trajectory, providing education and training of the philosophy, skills and knowledge in palliative medicine to medical undergraduates, basic trainees and higher trainees of other subspecialties, and promotion of palliative medicine through different platforms.20 Global atlas of palliative care at the End-of-Life (2014)The importance of collaboration between palliative care specialists and other health care professionals has also been stated in the Global Atlas of Palliative Care at the End-of-Life which describes palliative care provision at three levels: a “palliative care approach” adopted by all health care professionals, provided they are educated and skilled through appropriate training; “general palliative care” provided by primary care professionals and those treating patients with life threatening diseases, with a good basic knowledge of palliative care; and “specialist palliative care” provided by the specialised teams for patients with complex problems.21 Quality of death index (2015)In the 2015 Quality of Death Index by the Economist
Intelligence Unit, a survey ranking palliative care
across the world, Hong Kong ranked 22nd among the 80
countries surveyed, with a total score of 66.6 out of 100,
as compared with Taiwan’s score of 83.1. Hong Kong
did well in the affordability and quality of care domains
with scores of 82.5 and 81.3 respectively, reflecting the
achievement of the specialist-led palliative care services in
the public sector. However, there is room for improvement
in community engagement (score 32.5, rank 38), palliative
and healthcare environment (score 50.4, rank 28), and
human resources (score 62.1, rank 20).22 This report
highlighted several major areas for improvement in
order to meet the escalating needs of patients with life-threatening
illnesses: A recent research identifies the strengths and weaknesses as well as opportunities and challenges of palliative care services in Hong Kong. Despite high-quality services, comfortable environment, multidisciplinary team collaboration and committed staff in the specialist palliative care services, the limited coverage, inconsistent accessibility, fragmentation of care, delayed referral, lack of knowledge about palliative care in the general healthcare environment, inadequate coverage in professional education, lack of palliative care provision in primary care, and inadequate community and home care support are some of the obstacles to be overcome if all patients in need can receive appropriate palliative care. The study also identifies the barriers to palliative care development in the macro-environment including political, economic, socio-cultural, technological, environmental and legal aspects. (Figure 3) Five key principles for service development are recommended: fair access, compassionate care, early integration, shared decision-making, and continuity of care.23 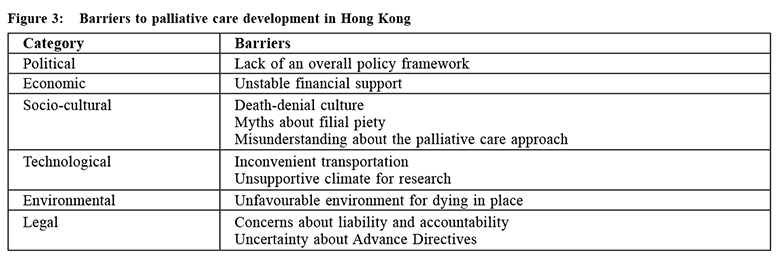
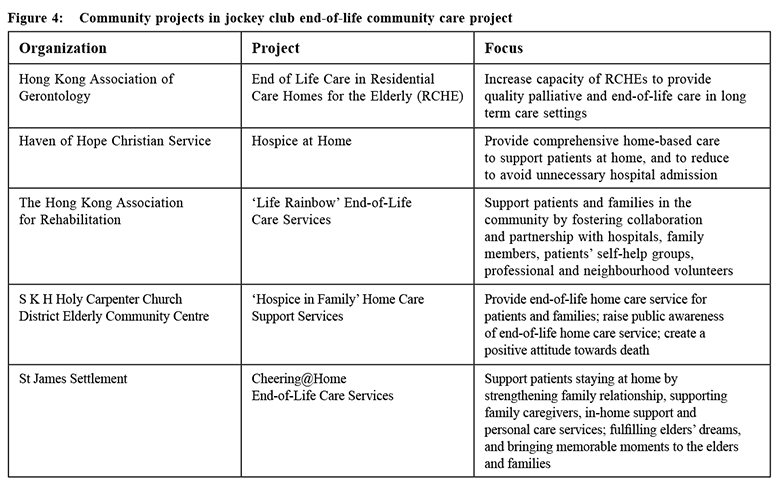
Strategic Service Framework for Palliative Care in Hospital Authority (2017) There are observable changes since 2015 pointing to improvement and opportunities in these areas of challenges and threats. The Hospital Authority has published its Strategic Service Framework for Palliative Care in 2017 which envisions that “All patients facing life-threatening and life-limiting conditions and their families / carers receive timely, coordinated and holistic palliative care to address their physical, psychosocial and spiritual needs, and are given the opportunities to participate in the planning of their care, so as to improve their quality of life till the end of the patients’ last journey”. The four main strategies for adult palliative care are: enhancing governance by developing cluster-based services with the collaboration of medical and oncology palliative care specialists, promoting collaboration between palliative care and non-palliative care specialists through shared care model according to patients’ needs, enhancing palliative care in the ambulatory and community settings to support patients and reduce unnecessary hospitalisations, and strengthening performance monitoring for continuous quality improvement. The key strategies of the Shared Care Model include needs stratification based on complexity so that less complex needs are served by parent teams and more complex needs are served by palliative care specialists, training and skills transfer of health care workers in non-palliative care settings, and strengthening specialist palliative consultative service to support the parent teams to provide palliative care to their patients. Besides palliative care for adults, development of palliative care service for children is another focus of the framework.24 Community projects and public awarenessThere are also changes in the community. In 2015, a three-year Jockey Club End-of-Life Community Care Project was kicked off which aimed to improve the quality of life of terminally-ill patients in the community, enhance the capacity of service providers and raise public awareness of the need of these services by trying different service models in the community run by several partnering non-governmental organizations (NGO). (Figure 4) This project is currently under evaluation to plan for the next step forward. Other NGOs like Society for Promotion of Hospice Care are also active in promoting palliative care in the community. Media coverage on needs of terminally ill patients, palliative care, and advance care planning / advance directive is also increasing. Interface between Primary Care and Palliative CarePrimary care contributes to the health of the population and covers a wide range of services which includes the delivery and provision of palliative care for disability or end-stage diseases.25 Primary care doctor can play an active and important role in palliative care in the following ways:
Currently, one can access via the Hospital Authority website to look for the appropriate palliative care service to be referred to in each cluster and to download the standard referral form. Referral criteria for the different palliative care services including in-patient, out-patient, day care, home care and inpatient consultative services are listed on the form. The link is: http://www.ha.org.hk/ visitor/ha_visitor_index.asp?Content_ID=1038&Lang=EN G&Dimension=100&Parent_ID=10096&Ver=HTML However, despite most family doctors agreeing that palliative care should be readily provided in the community, barriers hindering its development were identified in a local questionnaire survey of local members of the Hong Kong College of Family Physicians which included time concern, inadequate support from other disciplines, knowledge and experience, problems dealing with death, current public-private interface and cultural concerns.28 
Palliative Care Australia underlined three important elements to promote palliative care in primary care:
These elements are also relevant to Hong Kong to enhance palliative care provision in primary care setting, and networking and dialogue between palliative care and primary care doctors are essential. The way forwardIn the Policy Address of the Chief Executive of HKSAR in 2017, Item 163 was on palliative care development, signifying that the palliative care needs of patients was already on the agenda of the Government. In particular, the formulation of a strategic service framework on palliative care by the Hospital Authority, measures to enhance provision of palliative care and end‑of‑life care services within hospital settings and in the community, enhancing home care, training for the staff of residential care homes for the elderly, and Government’s consideration of amending the relevant legislation to give patients the choice of “dying in place” were mentioned in the report.30 Development of palliative care is a response to the suffering and unmet needs of patients with life-threatening illness in the modern health care system. It has been thirty-six years since the first palliative care service was established in Hong Kong. With the great efforts of the pioneers and the central coordination in the public hospital system, specialist-led palliative care service has benefited many patients and their families in need. However, to provide appropriate palliative care to all patients in need, it is time to review and revise our current approach. A territory-wide strategy should include legislation review, collaboration between palliative care specialists and other health care professionals through a shared care model as well as training and skills transfer, and enhancement of community engagement through collaboration with community partners and non-government organizations.
Wai-man Lam, MBBS, FHKAM, FHKCP, FRCP (Edinburgh)
Correspondence to: Dr. Wai-man Lam, Chief of Service, Department of Medicine,
Haven of Hope Hospital, 8 Haven of Hope Road, Tseung Kwan O,
Kowloon, Hong Kong SAR.
References:
|
|