|
June 2017, Volume 39, No. 2
|
Original Article
|
A Family Medicine specialist led diabetes mellitus clinic in a general out-patient clinicCP Lee 李植沛,SY Leung 梁淑茵,Maria KW Leung 梁堃華,Eric MT Hui 許明通,Philip KT Li 李錦滔 HK Pract 2017;39:38-42 SummaryObjectives: To evaluate whether adopting a Family Medicine specialist run diabetic clinic in a general outpatient clinic (GOPC) can improve standard of care of diabetic patients. Design: A prospective cohort study with before and after comparison. Subjects: All diabetic patients of the pilot GOPC. Main outcome measures: Primary outcome: Control rate of HbA1c, blood pressure and LDL cholesterol.
Secondary outcome: capture rate of clinical parameters, referral rate for Risk Assessment and Management Programme (RAMP), rate of statin use and rate of insulin initiation.
Results: 3,935 diabetic patients (94% of all diabetic patients in the pilot GOPC) were ecruited for analysis. Improvement was shown in various aspects, including LDL control < 2.6, HbA1c capture rate within 1 year, BMI capture rate within 1 year, rate of statin use, RAMP attendance and referral rate. However, BP control <130/80, HbA1c control < 7% and insulin initiation rate did not show statistically significant difference despite the trend in improvements seen. Conclusion: A Family Medicine specialist run diabetic clinic may improve the standard of care of diabetes mellitus patient in GOPC. Keywords: GOPC, diabetic clinic 摘要目的:評估家庭醫學專科醫生在普通科門診部主理糖尿病診所能否提升糖尿病人的醫療水平。 設計: 前瞻性群組性研究,比較在開設糖尿病診所前後的分別。
研究對象:所有在試點普通科門診內的糖尿病人
重要結果指標:主要指標:糖化血紅素、血壓和低密度膽固醇的控制比率。次要指標: 臨床指標的擷取比率,轉介往健康風險評估及跟進治療計劃的比率, 他丁類降脂藥使用率和開始使用胰島素治療的比率。
結果: 為共3 , 9 3 5名糖尿病人作分析,佔試點普通科門診內9 4 %的糖尿病人。結果顯示低密度膽固醇水平控制在 2.6 mmol/L 以下,一年內糖化血紅素擷取比率,一年內體重指標擷取比率,他丁類降脂藥使用率,健康風險評估及跟進治療計劃的出席及轉介比率均有明顯改善。可是,血壓能低於130 / 80 mm Hg,糖化血紅素控制於7%以下和開始使用胰島素治療的比率雖有改善,但未達到統計上的顯著差異。
結論: 家庭醫學專科醫生在普通科門診主理糖尿病診所或許可以提升糖尿病人的醫療水平。
主要詞彙: 普通科門診, 糖尿病診所 IntroductionDiabetes is a prevalent disease Diabetes mellitus (DM) is a chronic metabolic disease characterised by hyperglycaemia resulting from defects in insulin secretion and/or action due to interactions between genetic and lifestyle factors.1 Type 2 diabetes, being the most frequent form of diabetes among Hong Kong adults, is affecting around one in 10 people, or about 700,000 people.2 The prevalence rises from 2% in people aged less than 35 years to more than 20% in those older than 65 years.1,3 Diabetes is the leading cause of cardiovascular diseases, stroke, renal failure, blindness and leg amputations, becoming a continuous heavy burden to the healthcare system.4,5 The optimal control of blood sugar, blood pressure (BP) and lipid level in diabetic patients has been proven to reduce complications and is cost-effective in randomised controlled trials.5 Care of DM patients in GOPC Although guidelines on the management of diabetes in primary prevention of complications have been well established and widely disseminated, such as guidelines of American Diabetes Association, World Health Organisation and International Diabetes Federation, and American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Management of Diabetes Mellitus, many diabetic patients do not achieve optimal control according to the recommended targets. According to a local cross-sectional study launched in three GOPCs in Hong Kong involving 1,970 patients from July to October 2009, only 58.0%, 38.2% and 36.4% of patients achieved the glycaemic, BP and cholesterol targets, respectively.6 Another local research studying 127,977 diabetic patients under the primary care provided by the general outpatient clinic of Hospital Authority (HA) in 2013 revealed the control rates of clinical parameters were suboptimal, with 56.5 % achieving HbA1c < 7%, 56.5 % achieving SBP < 130 mmHg, 65.6 % achieving DBP <80 mmHg, while 62.5% achieving a low density lipoproteincholesterol (LDL) < 2.6mmol/L.7 A more recent local retrospective, population-based cohort study published in 2016 including all diabetes patients under the primary care services of Hospital Authority of Hong Kong also revealed similar findings, with 57.4%, 38.1% and 50.7% of patients achieving the HbA1c < 7%, BP < 130/80 mmHg and LDL < 2.6mmol/L targets, respectively.8 Therefore, it is worthwhile to explore whether a different care delivery model in GOPCs is able to improve the standard of care for DM patients. Risk Assessment and Management Programme In August 2009 , HA implemented a multi - disciplinary Risk Assessment and Management Programme (RAMP) to improve the quality of care for patients receiving diabetic care in the GOPCs.9 The programme adopts a standardised protocol consisting of a workflow of measuring relevant clinical parameters including HbA1c, blood pressure, LDL, and an agreed risk assessment criteria for risk level stratification. All patients enrolled in the programme would undergo a comprehensive risk assessment and screening for diabetes-related complications, and are then assigned to different management options according to the their stratified risk level, including appropriate interventions and education provided by a team of multi-disciplinary healthcare professionals. Family Medicine Specialist The GOPC service in HA is currently supported by doctors with different training backgrounds, including Family Medicine (FM) Specialists, FM basic and higher trainees as well as service doctors who are not undergoing the FM training. A FM Specialist holds a statutory professional qualification with defined requirements.10 FM specialty doctors will go through a 4-year Basic Vocational Training and pass the Hong Kong College of Family Physicians (HKCFP) / Royal Australian College of General Practitioners RACGP (RACGP) Conjoint Examination. Then they can proceed to a 2-year Higher Training in FM and if they pass the Exit Examination, they are eligible to be admitted as Fellows of the Hong Kong Academy of Medicine and hence will be registered as Specialists in Family Medicine by the Medical Council of Hong Kong. This training programme prepares doctors to provide highquality specialist care to the community as a family physician. A minimum period of four years is deemed necessary for the basic training in FM because this discipline requires a broad knowledge and skill base. It also requires extensive clinical exposure in order to develop the necessary attitudes appropriate for a primary care physician. One study found that FM specialists practice was perceived to be safe and able to provide effective treatments in a challenging medical discipline that was in line with the current standards of medical care and ethical and professional values.11 This study tries to explore whether Family Medicine Specialist can deliver a high standard of care to DM patients.Specialist Diabetes Mellitus Clinic A diabetic clinic run by Family Medicine specialists was piloted in a general out-patient clinic (GOPC) in order to evaluate whether it can show improvement in the standard of care of diabetes patients in a primary care setting. MethodStudy design To have a diabetic clinic run by a team of Family Medicine specialists piloted in a selected GOPC in the New Territories East Cluster of Hong Kong set up since September 2014. All the existing diabetic patients from different consultation rooms of the pilot GOPC were recruited into a diabetic clinic which consisted of a single consultation room located in the same GOPC attended by a FM specialist from Monday to Friday 09:00-17:00 and Saturday 09:00-1300. This clinic had exactly the same setting as other consultation room in the pilot GOPC, with a slightly reduced case load as compared to a usual GOPC quota (35 vs 40 patients in a 4-hour morning session, 25 vs 30 patients in a 3-hour pm session). No additional clerical and nursing support was provided and the drug list was that of the existing the pilot GOPC’s formulary. All patients with a clinical diagnosis of Type 1 or Type 2 DM, and having regular follow up in the pilot GOPC were included in the study. DM was identified with the International Classification of Primary Care (ICPC) code of ‘T89’ or ‘T90’ through the Clinical Management System (CMS) database of HA. Clinical data from all these diabetic patients before and after the establishment of the DM clinic in September 2014 was analysed and compared using McNemar’s test for proportion of patients treated to targets. Relevant socio-demographic data was retrieved from central CMS of HA database. (Table 1) The primary outcomes include the control rate of blood pressure < 130/80 mmHg, HbA1c < 7% and LDL < 2.6mmol/L. Secondary outcomes include the capture rate of HbA1c and body mass index (BMI) within 1 year, rate of statin use, rate of insulin initiation, RAMP referral rate and RAMP attendance rate, were retrieved through the Clinical Data Analysis and Reporting System (CDARS) of Hospital Authority. 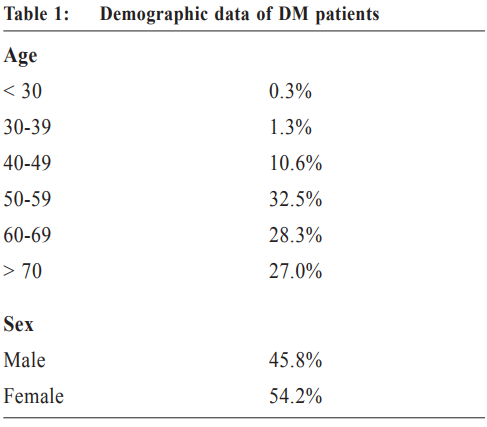
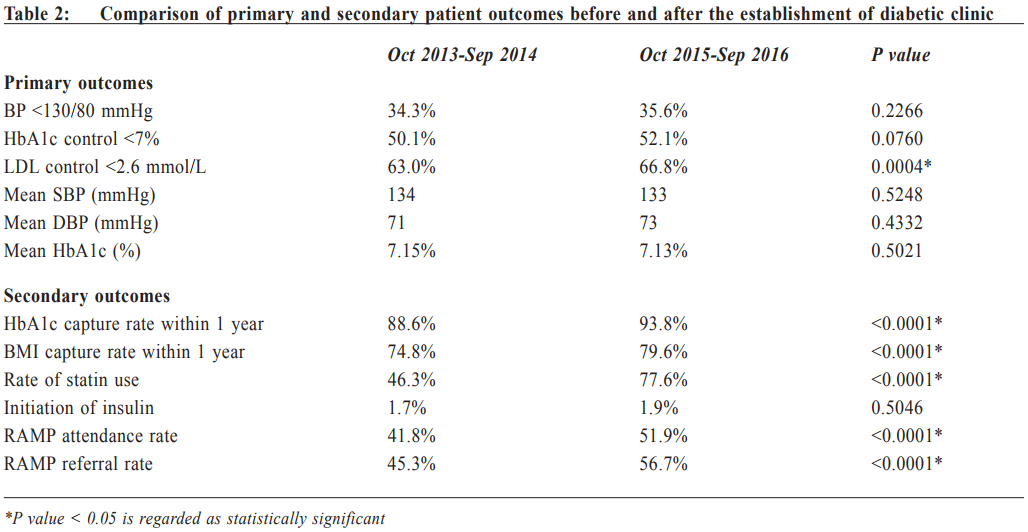
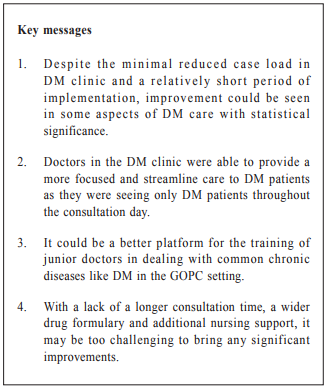
Results3,935 diabetic patients were recruited under the care in the diabetic clinic, which covered 94% of all DM patients of the pilot GOPC. 54.2% of diabetic patients were female while 45.8% were male. Around 90% of patients were more than 50 years old, with around one third were 50-59 years old, roughly one forth were 60-69 and one forth were more than 70 years old (Table 1). The remaining 218 patients were not recruited into the diabetic clinic, which comprised 6% of our total diabetic patients. Among these 218 patients, 79 (36%) were new cases which were pending for recruitment in subsequent visits, 69 (32%) were defaulted cases of diabetic clinic, and 13 (6%) were not diabetic patients with a wrong ICPC code. Only 47 (22%) patients were transferred back to original consultation room after recruitment into the diabetic clinic due to patient preference. The remaining 10(4%) cases were diabetic patient under regular follow up in other department. Data from October 2015 to September 2016 (after the establishment of the diabetic clinic) was compared to those from October 2013 to September 2014 (before the establishment of the diabetic clinic). Statistically significant improvement was shown in various aspects, including LDL control < 2.6 (63.0% vs 66.8%, p=0.0004), HbA1c capture rate within 1 year (88.6% vs 93.8%, p < 0.0001), BMI capture rate within 1 year (74.8% vs 79.6%, p < 0.0001), use of statin (44.6% vs 77.6%, p < 0.0001), RAMP attendance rate (41.8% vs 51.9%, p < 0.0001) and RAMP referral rate (45.3% vs 56.7%, p < 0.0001). However, there was no statistically significant improvement in other clinical parameters, including BP control < 130/80 (34.3% vs 35.6%, p=0.2266), mean systolic BP (SBP) (134 vs 133, p=0.5248), mean diastolic BP (DBP) (71 vs 73, p=0.4332), HbA1c control < 7% (50.1% vs 52.1%, p=0.0760), mean HbA1c (7.15% vs 7.13%, p=0.5021) and initiation of insulin (1.7% vs 1.9%, p=0.5046). (Table 2) DiscussionDespite the minimal reduced case load in DM clinic and a relatively short period of implementation, improvement could be shown in some aspects of DM care with statistical significance, including LDL control < 2.6, HbA1c capture rate within 1 year, BMI capture rate within 1 year, use of statin, RAMP attendance rate and RAMP referral rate. There was no statistically significance improvement in BP control < 130/80, mean SBP and DBP, HbA1c control < 7%, mean HbA1c and initiation of insulin. The improvement in standard of care in DM patients delivered by this modified care delivery model in GOPC may be due to several factors. Firstly, doctors were able to provide more focused and streamline care to DM patients as they were seeing only patients with DM throughout the consultation day and this may explain the RAMP referral rate and attendance rate were better after set up of the diabetic clinic with statistically significance. Secondly, Family Medicine specialists were well trained to take care of the other co-morbidities. DM patients have and can present with other episodic illnesses within the same appointment setting similar to the usual GOPC setting. Even though there was no difference in restriction of prescribing statin between GOPC and diabetic clinic, the rate of statin use was significantly higher in those who attend the diabetic clinic. Thirdly, as some of the DM patients in the pilot clinic were under the same doctors’ care for many years previously, change of the attending doctor may help to break the clinical inertia, so that patients who refused change in their treatment regimen might be motivated by seeing a “new doctor” in the diabetic clinic. Besides, the slight quota adjustment may allow doctors to have more time in building rapport with the patients and allow more time for assessment and explanation of treatment plan, though on average only 1 minute per patient more consultation time was gained after the quota adjustment. Furthermore, it can also be a better platform for the training of junior doctors and trainees in dealing with common chronic diseases like DM. Trainee can be arranged to attend one single training session in the diabetic clinic, then they have the opportunity to appreciate the clinical skills in handling a wide spectrum of diabetic patients of different severity, from newly diagnosed diabetes, diabetes on diet control only, to patients with a long standing history of diabetes on insulin therapy, which may not be feasible in the usual setting of a general out-patient clinic. However, there may be some drawbacks for this new DM care model. As all DM patients with potentially more co-morbidities were managed in the same session in the diabetic clinic, while ordinary GOPC would encounter patients with less complicated cases, e.g. hypertension, hypothyroidism, or episodic illness like upper respiratory tract infection only. Without a longer consultation time as there was only a slight reduction in quota, without wider drug formulary (no newer generation of oral hypoglycaemic agents were available in the diabetic clinic), without additional nursing support, were referred for RAMP as usual in GOPC without any early appointment availability or a more flexible appointment arrangements, it may be too challenging to bring significant improvement within a relative short period of time by handling all DM patients together.
Moreover, as the period of the establishment of the diabetic clinic is still short, in order to accommodate all the existing DM patients in the pilot GOPC into a single room without additional session, by the time of evaluation of the various clinical parameters in this study, patients were seen by FM specialists for around 6-7 times only with the average follow up period varying between 14-16 weeks, some of the patients may need more time to accept further lifestyle modification or adjustment of their existing drug regimen in order to bring significant improvement in various clinical parameters. The fluctuation in blood pressure control after the initial intensification treatment may also result in the suboptimal improvement in meeting the blood pressure target in these patients. A longer review time may be necessary to see the effects of adopting this new care of model. ConclusionThere was a statistical significant improvement in some aspects of the standard of care of GOPC DM patients after establishment of the FM specialist run DM clinic. Further study on its long term effect is needed. CP Lee, MBChB (CUHK), FRACGP, FHKCFP, FHKAM (Family Medicine) Correspondence to: Dr CP Lee, Department of Family Medicine, Prince of Wales Hospital, New Territories, Hong Kong SAR, China.
References
|
|