|
September 2016, Volume 38, No. 3
|
Discussion Paper
|
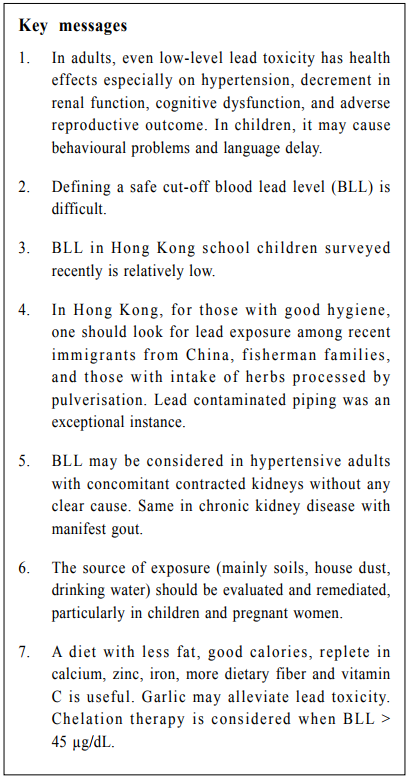
Hong Kong lead burden: control in the recent decadesEdwin CL Yu 余秋良,CB Chow 周鎮邦 HK Pract 2016;38:93-100 Summary Silent lead exposure has many long-term consequences. Changes in tightness of control and the recent lead-related incidents in Hong Kong are described. Based on world standards, health actions by our medical profession are proposed. According to current standards, blood lead level (BLL) > 5 μg/ dL justifies providing information to families on lead hazards and on the usual sources of uptake, as well as close biological surveillance along with hygiene and dietary advice aiming at reducing contact. Sources of exposure should be investigated and avoided, particularly for children and pregnant women. In children, developmental surveillance should be performed during medical visits. A diet with less fat, good calories, replete in calcium, zinc, iron, more dietary fiber and vitamin C helps. Garlic may alleviate lead toxicity. Chelation therapy should be considered when BLL > 45 μg/dL. 摘要 自1970年,對鉛毒的意識開始普及。有關曝露於鉛污染後 對神經及其他系統影響的瞭解和研究日益增加。在不知曉 的情況下接觸鉛污染會引起多種長遠後果。本文敘述對管 制鉛量尺度的轉變,及近日在港發生與鉛毒相關的事件。 本地醫學界已按照國際標準訂出在健康行動上的建議。依 據目前準則,當血鉛量>5微克/分升時,會向有關家庭成員 提供鉛害資訊,講解常見吸收鉛的來源,為他們提供緊密 的生理監察及在衛生和飲食上的忠告,旨在減少他們繼續接觸。對鉛的源頭(主要是土壤,家居塵埃,飲用水)應 該進行調查,並著意避開,尤以兒童及孕婦為甚。兒童應 在日後就診時進行智能發展監察評估。日常飲食應少含脂 肪,有充份的熱量、鈣、鋅、鐵及較多的膳食纖維和維生 素C。進食大蒜或可減輕鉛的毒性。當血鉛量>45微克/分升 時,應考慮施以螯合療法治療。 lntroduction Lead (Pb) is a well known neurotoxic agent with lasting adverse health effects. In the recent decades, authorities have moved from investigational standpoints to proactive assertiveness for control. Primary and secondary prevention of associated neurodevelopmental and behavioural disorders need cooperation between parents, clinicians, and educators in Pb poisoning prevention programmes, an idea that was exemplified by the Centres for Disease Control and Prevention (CDC) Advisory Committee on Childhood Lead Poisoning Prevention in 2008.1 The neurological effects of Pb poisoning range from behavioural issues (e.g. emotional lability, attention deficit disorder with hyperactivity, or anxiety), pervasive developmental delay particularly in language, to encephalopathy. In utero, Pb exposure adversely affects infant neurodevelopment, besides possible low infant birth weight, miscarriages or premature birth. Neurobehavioural effects of Pb poisoning can persist into adolescence despite a decline in BLL. Neurological effects include hearing loss, peripheral neuropathy, and decreased nerve conduction velocity. Pb encephalopathy in patients may also be associated with partial heart block and deterioration in renal function. Effects of lower asymptomatic blood lead levels Awareness into the long-term consequences of Pb exposure has grown since 1970. Young children with high BLL have impaired intellectual functioning and behavioural problems that lasts a lifetime. Pb exposure is associated with antisocial behaviour like murder, crime, and aggressive behaviour. In 1991, the United States Public Health Service Strategic Plan called for a society-wide effort to eliminate childhood Pb poisoning within 20 years. At that time, the allowed BLL was up to 10 μg/dL. Subsequent studies demonstrated that even lowlevel Pb exposure significantly impairs learning and educational attainment.2-8 Newer studies showed that BLLs between 2-10 μg/dL result in cognitive deficits in children and adolescents, with an inverse relationship between BLL and performance on arithmetic and reading2, intellectual impairment in children3, and specific attention effects in young children.4,5 Finally in 2012, CDC used their population’s 97.5th percentile’s BLL of 5 μg/dL as the reference upper limit in young children.9 Pb persists for long periods in our body, with a half-life of 25 days in blood, 40 days in soft tissues, and 20 years in bones. Thus a mother with Pb accumulation could release it to the foetus during pregnancy. Pregnancy increases mobilisation of Pb from maternal skeleton.10 In utero exposure to Pb adversely affects infant neurodevelopment independent of postnatal BLL. Adults may be affected in other ways. Pb exposure is associated with telomere length shortening11, an indicator of aging. In the elderly, the risk of dementia increases with Pb burden.12 Pb has effects on renal function, and is epidemiologically related to hypertension.13 This was demonstrated for high BLL14 and also for BLL < 10 μg/dL. Bone Pb level was better correlated with hypertension15 suggesting that the hypertensive effect of Pb may depend on the cumulative lifetime Pb dose. Various actions on lead control Pb may be absorbed through the gut and skin, and also be inhaled. Absorption is much more efficient in children (~50%) than adults (~10%). Among children, 55% of Pb comes from dust and soil, 20% from food, 15% from air, and 10% from water and other sources. Adults should consider food, beverages, and herbs as sources. Young age in children, poor nutrition and lower socioeconomic status are clearly associated with chronic Pb poisoning.16,17,18 In addition, chronic exposure runs the greatest risk for neurological consequences. An analysis of trends in BLL over the past 20 years shows that, although the overall geometric mean BLL in children has dropped dramatically, certain populations are still at increased risks. A survey in 1998 on 457 Chinese new immigrant children showed that 18.1% had BLL > 10 μg/dL and 2.6% > 15 μg/dL within 7 days of arrival to Hong Kong. 93% with initial high BLL experienced reduction in levels after staying 2-3 months in Hong Kong19, demonstrating the significant Pb burden in China. Researchers from Greenpeace and International POPs Elimination Network (IPEN) bought 500 toys and children’s products from five Chinese cities including Beijing, Shanghai and Hong Kong and, after testing them with hand-held X-ray scanners, found that 32.6% were tainted with heavy metals.20 Advocates proposed that regulatory policies need to be put in place in China in order to reduce Pb emissions from numerous Pb-related industries, to develop new and renewable energy sources away from coal consumption and thermo-power-generation processes, and to improve quality control systems for BLL screening and testing.21 The Hong Kong scene Unleaded petrol was introduced to Hong Kong in April 1991. In 1998, sales of unleaded petrol comprised over 90% of the market. Gazetted through the Environmental Protection Department, the sale and supply of Pb-gasoline was banned since 1 April 1999. Also, a guidance note was given on the best practical means for Pb control: a green procurement page with a list of 103 government procurement products that follows Restriction of Hazardous Substances (RoHS) and Community and Public Sector Union (CPSU) was made available for the business sector to follow. Amendments to the Toys and Children’s Products Safety Ordinance in 2013 adopted the most up-to-date standards for various products including children’s paint. The Government health, food and environment, and civil engineering departments were all vigilant about possible high Pb consumer products. Regular education pamphlets on dietary and environmental education to avoid Pb exposure have been made. However, the regulation is a retrospective one and recall action will only be taken upon complaints or products found to be unsafe. The high mean Pb levels in outdoor roadside dust and coastal waters noted in 1990 and 1998 studies were much lowered from those 10 years ago.22,23 General decrease in roadside dust Pb over the 1990’s had been related to the reduction in petrol Pb level.24 Indoor Pb levels studied in 1997 in nursery schools and kindergartens territory-wide25 showed floor-dust Pb worst in North Point and Kwun Tong. Floor-dust in schools close to freeways, to gas stations and to factories had higher Pb. Use of vacuum cleaner was effective in reducing Pb. Generally, drinking water in Hong Kong has been thought very safe for Pb.19 Yet there are no legislation and regulation on Pb in paints. Customs department (C&ED) only advised manufacturers to put on the warning level if paints confirmed Pb levels exceeded. The Choice Magazine in 2002 and 2014 found that Pb concentrations in some paints to be around 21-28 ppm, while some were as high as 36-38 ppm. Investigation by Greenpeace East Asia and IPEN in 2011 on 25 kitchen products (mainly ceramic mugs and painted glasses) sold in Hong Kong showed that 52% contained Pb at levels greater than the 90 ppm recommended standard. Ten of these Pbcontaining products has levels of >10,000 ppm, more than 100 times the 90 ppm standard. Two glasses contained more than 40,000 ppm Pb. The prevalence of high BLL was investigated in a school study by the University of Hong Kong in 1984. The mean BLL among 5,608 students aged 6-17 years was 14.0 ± 5.1 μg/dL (17-45.0 μg/dL), similar to or lower than those in large cities.26 A remarkably high prevalence was suggested by a community-based (Kwai Tsing) convenient sample of 101 children who participated in the Telehealth project 2000-2001. Using blood and occipital hair Pb (PbH) as samples, the mean BLL was 6.52 ± 5.0 μg/dL (0.51-25.9 μg/dL) and 18.2% had levels > 10 μg/dL.27 None had related symptoms. 6.2% had PbH above the harmful level of 11 μg/g. A risk assessment questionnaire noted lowered economic status and age below six as risk factors. Peeling paint chips and second hand cigarette smoke from household member were significantly correlated to PbH level. In another study in 201228, BLL was found to be dependent on gender and residential district. Students from schools of lower academic grades had higher BLL, while BLL was higher in the New Territories and lowest in Hong Kong Island. Urinary albumin was positively associated with urinary Pb. A larger study is needed to make definite conclusions. The intake of Pb through the intestinal route had been scrutinised. A Baptist University study in 1996 on local and imported vegetables found Pb levels to be below the maximum permitted level.29 In 2005, the Food and Environmental Hygiene Department found high Pb levels in vegetables and seafood. On the other hand, low levels of Pb was detected in cereal and cereal products, fruits, meat, poultry, eggs and their products. Levels were undetectable (< 0.3 μg/kg) in “milk and dairy products”.30 The dietary Pb exposure was estimated to be 1.98 μg/kg bw/wk. Pb from “vegetables” could contribute to 57.7% of the total exposure. Nevertheless, this was accepted as well within the laxer standards that time. Soaking and washing vegetables thoroughly to remove dust and soil can drastically reduce Pb concentration. Lime preserved eggs and oysters were found to contain high Pb concentration in this report, but it actually depends on the manufacturer. Recent social disaster from leaded water In Hong Kong, Pb poisoning prevention has been thought as a success. In fact, Hong Kong in recent years has followed the world climate and made regulations even without much local studies for support. Water has all along been considered safe until recently. Hong Kong started receiving Dongjiang water from China in 1964, and water quality throughout the supply system has always been systematically and regularly monitored at representative sampling points to have comprehensive and stringent monitor. In Hong Kong, Pb pipes have been banned since the 1930s (other countries such as United Kingdom and United States of America banned them since 1970s-1980s). Childhood plumbism has long been done away as galvanised iron (GI) and copper pipes are used. Given the precautionary measures instigated in Hong Kong the recent Pb-tainted water issue thus came as a surprise, and highlighted the difficulties in identifying the root Pb source. In the United States of America, the use of Pb-based soldering of copper pipes was permitted until 1986, and currently older housing homes in poverty may still have substantial Pb in the water. Since July 2015, on-site evaluations in our locality involved screening for Pb in estate water samples. Subsequent investigations were redirected to find out the various ways in which drinking water can be contaminated after entering a building.31 Of greater concern, however, is the risk of adverse cognitive effects from low BLL in children. Currently, the Joint Food and Agriculture Organisation of the United Nations FAO/WHO Expert Committee on Food Additives (JECFA) concluded in 2010 that it was not possible to establish a threshold Pb levels for the neurological effects in children. The Committee carried out a dose response analysis and reported that a Pb exposure level of 0.3 μg/kgbw/day (2.1 μg/wk) was associated with a population decrease of 0.5 IQ points. Now, research shows that no safe BLL has been identified. The European Food Safety Authority (EFSA) Panel on Contaminants in Food Chain32 concluded that there is no threshold Pb levels for developmental neurotoxicity in young children, nephrotoxicity and cardiovascular effects in adults (associated with BLL 0.5 μg, 0.63 μg and 1.5 μg/kg/day respectively). To note, in the United States, the average BLL in unexposed individuals is 3 μg/dL. Public health actions and target lead level With no safe Pb level limit, rigorous reduction in environmental Pb (e.g. in soil, dust, air and industrial products) is imperative, especially for young children and unborn babies. The childhood BLL reference (currently 5 μg/dL) used by the CDC is within two standard deviation range of the population-BLL among children aged 1-5, and helps to identify children and environments associated with Pb-exposure hazards. The reference value will be updated every 4 years based on the most recent BLL population surveys.33 The Australian National Health and Medical Research Council recommended that: a) BLL > 5 μg/dL suggests past or on-going Pb exposure at a level above what is considered the average ‘background’ exposure, b) for BLL > 5 μg/dL, the source of exposure should be investigated and reduced, particularly if the person is a child or pregnant woman, c) individuals should have their BLL tested if they have swallowed or breathed Pb from a particular source or someone in their household has had BLL > 5 μg/dL; or they have unexplained health problems that could be due to Pb.34 In France35 , environmental Pb exposure is considered likely if BLL > 25 μg/L, when information on Pb hazards and potential sources of uptake should be given to families. In addition, close biological surveillance along with hygiene and dietary advice aiming at reducing contact should be instigated. These new reference levels will have to be updated every 10 years. Alert values are also proposed for the main sources of Pb in the environment (soils, house dust, tap water). Mandatory screening or identification of high risk groups is performed in Connecticut of the United States. CDC and France also recommend screening for Pb exposure using environmental risk standards developed locally. Medical actions Physicians should offer health-based recommendations on the management of Pb-exposed individuals aimed at primary and secondary prevention of Pb-associated health problem. While much may be public health or educational concerns, doctors may in time need to support school-based health services to children and adolescents including routine and preventive screenings and examination including BLL and follow-up, diagnosis and treatment of acute uncomplicated problems, and monitoring and treatment of chronic medical conditions. BLL has now become more readily available in clinics. Diagnosis requires a high index of suspicion. Evaluations for neurophysiological and renal dysfunction should be performed. Characteristic features include abdominal colic, anaemia with basophilic stippling of red cells, gingival Pb lines and dense metaphyseal lines in X-ray. Chronic Pb toxicity often present with non-specific symptoms and may be easily missed. In children, these include temperamental lability, irritability, behavioural changes, hyperactivity or decreased activity, delayed developmental milestones and language delay. Blood samples are useful for testing for Pb exposure.36 Technology now allows testing of hair, teeth, or fingernails for Pb, radiographic imaging or X-ray fluorescence of long bones, and other tests for chronic exposure. By X-ray excitation of electrons in the K shell of Pb atoms, the K-line radiographic fluoroscopy permits detection of Pb molecules from the full thickness of bone and allows accurate assessment of the Pb-to-calcium ratio. Radiographic fluoroscopy is safe, noninvasive, and reliable. Although occupational and household risks (except some kitchen wares and toys) are minimal in Hong Kong, herbal consumption remains our main concerns. To note, Pb contamination of herbs is mainly due to its processing with grinders and pans during pulverisation, not so much with raw herbs or herbal granules made from extraction. Fisherman families are another concern. Chronic low to moderate levels of Pb exposure in adults can result in four main categories of health effects, namely hypertension, decrement in renal function, cognitive dysfunction, and adverse reproductive outcome. Chronic Pb nephropathy as a progressive interstitial nephropathy has no characteristic findings. Most patients are hypertensive at diagnosis. It is usually the result of years of repetitive or continuous Pb exposure and thus tends to manifest in adulthood. Clinically, hypertension is too common to indicate Pb screening, but finding moderate-toconsiderable contraction of kidneys without any clear cause should raise its suspicion. Concomitant gout (not just hyperuricemia) is particularly noteworthy. More than 50% of patients with Pb nephropathy manifest as saturnine gout. Even though hyperuricemia is universal with renal insufficiency, gout is rare unless the patient has underlying Pb nephropathy. In fact, tests for estimating Pb burden should be considered in every patient with the combination of chronic kidney disease and gout.37
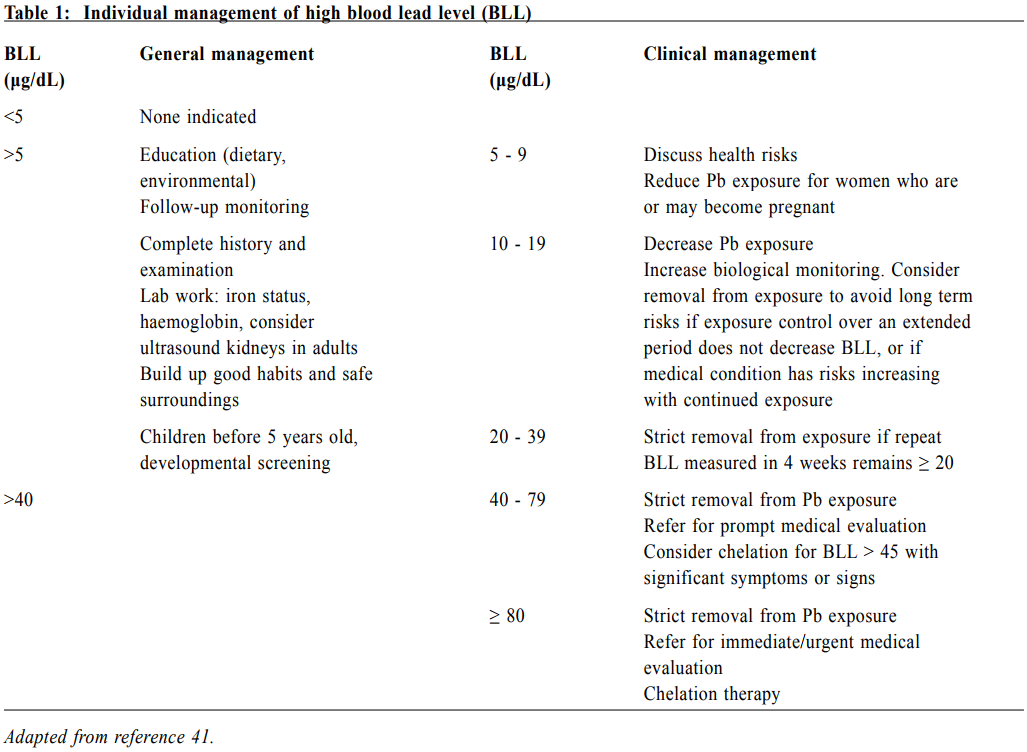
Table 1 outlines the measures physicians should take in order to manage patients with raised BLL. Termination of Pb exposure is imperative. The source of exposure (mainly soils, house dust, drinking water) should be investigated, particularly in children and pregnant women. BLL correlates best with recent exposure (remote exposure not excluded). The best measure for assessing total body Pb accumulation is the Ethylenediaminetetraacetic acid (EDTA) Pb-mobilisation test. For epidemiologic screening of large populations, the K-line radiographic fluoroscopy allows accurate Pb assessment of full thickness of bone, while the Pbcalcium ratio has been proposed as a biomarker of longterm cumulative Pb exposure. Diet is important in Pb management. Pb absorption is increased when a diet rich in fats is consumed. Also, diets low in iron, calcium, and vitamin C increase the likelihood of Pb absorption. Dietary fiber promotes good peristalsis and helps decrease Pb absorption. A recommended diet should be adequate in energy (caloric) intake and rich in calcium, zinc, and iron. Data from the Normative Aging Study suggest that low vitamin D intake may increase Pb accumulation in bones, whereas low vitamin C and iron intake may increase BLL in middle-aged to elderly subjects.18 The American Academy of Paediatrics recommends conducting annual developmental surveillance for children with a BLL ≥ 5 μg/dL at any age, aiming to identify emerging or unaddressed behavioural, developmental and cognitive problems.1 Five classes of Pb toxicity have been identified by the CDC:
Evidence suggests that chelation therapy for BLLs < 45 μg/dL can be potentially harmful.38 All affected individuals should have Pb prevention education, also identifying and eliminating other possible Pb sources. While chelation therapy is not without potential risks, garlic has been tested experimentally39 and shown to significantly reducing BLL, has less side effects and results in clinical improvement.40 Though larger studies are required to make a general conclusion, garlic is worth using for less toxic cases. Other lifestyle measures can also be considered, including the washing of hands, toys and vegetables, cleaning dusty surfaces, running cold water for one to two minutes before using, preventing children from playing on soil, eating a healthy diet, and being careful where one eats (Appendix). Secondary prevention programmes can be offered to those affected.1 Development can be usefully promoted by provision of a nurturing and stimulating family environment. Conclusions BLL below 5 μg/dL is taken as the action level, though even low-level Pb toxicity has health effects in adults and in children especially. Control recommendations by advocacy groups have become proactive. Local studies are needed to substantiate proactive claims. The recent Pb-tainted water issue demonstrated how one might overlook hidden Pb sources. In patients with Pb toxicity, doctors could offer help with environmental and medical preventive actions, health-based recommendations aimed at primary and secondary prevention of Pb-associated health problems. Acknowledgement Thanks to Dr Addi Chan for offering material information.
Edwin CL Yu, FRCP, FHKAM
ReferencesCroucher Fellow, Honorary Professor School of Chinese Medicine, Hong Kong Baptist University CB Chow, MBBS, FHKCPaed Honorary Clinical Professor Department of Paediatrics and Adolescent Medicine, The University of Hong Kong Correspondence to: Dr Edwin CL Yu, Rm 1901-03, Chung Kiu Commercial Building, 47-51 Shantung Street, Mongkok, Kowloon, Hong Kong SAR, China. E-mail: yuedwin@yahoo.com
|
|