|
June 2016, Volume 38, No. 2
|
Letters to the Editor
|
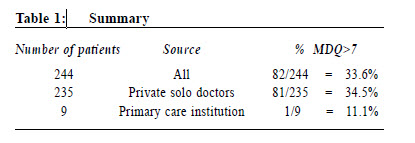
Letters to the EditorDear Editor, On a second bipolar study After the publication of the study on “the prevalence of bipolar disorders among Chinese adult patients seen in Hong Kong’s primary care clinics suffering from depressive illness” during the period October 2008 to April 20091, the present writer planned a second study on depressive patients who were treated in Hong Kong’s primary care community, but included both private solo primary care doctors and primary care institutional doctors. The objective was to assess whether there was any difference in the prevalence of bipolar disorders among depressive patients in these two categories. Patients were recruited with the same criteria of the previous study.1 The recruitment was done from year 2010 to 2013. The period was much later than the previous study because I had to write a number of documents to the ethical committees and to get approval of recruitment of patients from the primary care institutions. Results and analysis I got 284 patient cases in total. With exclusion of 13 cases which were not valid for study and 27 cases of public primary care institutions who withdrew themselves from the study, I finally had left with 244 patient cases entered for analysis. 9 patients were from a private primary care institution and 235 patients from various solo private doctors. 82 patients had scores of more than 7 in the MDQ (Table 1). The result of 33.6% means a prevalence of about one in three cases of depressed patients tested positive for having bipolar disorder. The prevalence in a primary care institution is 11.1%, and in the private doctors is 34.5%. Discussion This is the first study that involves primary care institutions. Although this study is truncated and sample size is small, it shows a significant difference in prevalence in bipolar disorder in solo private doctors (34.5%) and primary care institutions (11.1%). Both are primary care and the difference might be explained by patients’ preference. Solo private doctors might provide more privacy, convenience and personal care. The three private doctors, who contributed their cases in this study, have great interest in mood disorder, having a lot of depressive patients. This explains why the result (34.5%) is higher than the previous study (20.9%).1 Various international studies also show a big variation in prevalence (21.3% to 49%)2,3 in different clinical settings. Prevalence of 11.1% in a primary care institution should not be ignored. That means we might miss 1 bipolar patient in every 11 depressive patient. Interestingly that the prevalence rate in the primary care institution, withdrawn from the study, is also 11.1%. Many doctors made the clinical diagnosis of major depressive disorder and resistant depression4,5 without ruling out bipolar depression, and perhaps prescribed strong antidepressant which might trigger a hypomanic/manic episode and rapid cycling.6 I hope this letter will raise primary care doctors’ awareness of bipolar disorders.
Acknowledgements I wish to thank the following participating institution : general out-patient clinic, Hong Kong Sanatorium and Hospital; and participating doctors, Drs. Law Sai On, Tam Chi Wing and Wong Wing Ling.
Mary BL Kwong, MBBS (HK), FRCP (Edin), FHKAM (Paediatrics), FHKAM
(Family Medicine)
Specialist in Paediatrics
References
|
|