|
September 2015, Volume 37, No. 3
|
Dr Sun Yat Sen Oration
|
Making a difference: a journey in family medicineDonald KT Li 李國棟 HK Pract 2015;37:109-117 President and Council Members of the Hong Kong College of Family Physicians, President of the Royal Australian College of General Practitioners, Fellows, Members, New Fellows, Distinguished Guest, Ladies and Gentlemen: It gives me great pleasure to deliver this 26th Dr Sun Yat Sen Oration, and to witness the College’s 28th Fellowship Conferment Ceremony.
It is a special honour for me to speak here, myself being a Family Physician, in private medical practice, a Fellow of this College, and currently President of the Hong Kong Academy of Medicine. My journey to this point is perhaps symbolic of the increasing respect and recognition within the professional and wider community that our specialty has steadily been gaining in Hong Kong. And, in turn, it reflects the evolving status and leadership role of our unique specialty worldwide. Individually and collectively, Family Physicians can enjoy a satisfying and fulfilling career. Those reaching a milestone in their professional journey tonight as new Fellows have much to celebrate. But the future holds many challenges. Doctors have to work harder than ever before to stay at the forefront of their fields and to earn trust from their patients, especially owing to the fast pace of changing public perceptions and evolving technology. Now, straight away, I can attest to the new graduates of the College that it is true that you never stop learning, and indeed you cannot ever stop learning. This has become increasingly important since the start of this new millennium, as many professions worldwide, including Medicine, have made Continuing Professional Development compulsory and emphasised the need to personally take regular stock of your learning goals and achieved outcomes. Doing so helps you develop personally and helps your profession gain respect and continue to address expectations from patients, society, and government. As Academy President for more than 2 years and in my capacity before that as President for the Asia Pacific Region for the World Organisation of Family Doctors, I have been fortunate to attend conferences in all corners of the globe. In my travels to both developed and developing nations, not only have I myself learnt professionally from various educational meetings, but I have also learnt from being exposed to different cultures and from seeing how things are done in different places. In particular, I have keenly observed the commonalities and differences in health care systems, as well as in the training and continuing education of medical professionals and especially Family Physicians. I have learnt about what has worked well and what has not worked so well, and it has been my duty to constantly think of ways of applying what I have learnt to the communities I serve.
Tonight, I would like to share with you some insights of my professional journey so far, and what I have noticed in the changing relationship between Family Medicine and various aspects of our complex environment. What is clear to me is that much has changed since I first started learning Medicine in the 1970s. I can indeed conclude the only constant thing is change . Once qualified , we cannot be complacent, storage vessels of knowledge and wisdom. Technological, cultural, and demographic developments are among the many factors that have a considerable influence on how we practise Family Medicine, how our value is perceived, who our patients are, why they present to us, and what they expect. We must be engaged, proactive, and adaptive in order to keep being efficient and effective in making an observable and measurable positive difference in our communities.
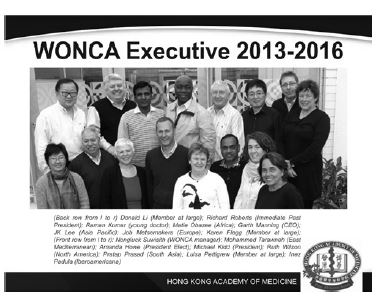
It was, in fact, in the 1970s that the world really started to pay attention to Family Medicine and its importance in helping to achieve equity in health care. The World Organisation of Family Doctors or WONCA was established in 1972 to represent our profession internationally and to raise its profile such as by interacting with the World Health Organisation. As a member of WONCA’s current Executive Committee as its Member-at-large, I proudly act as an advocate to unite our voices and aims, and for our College to fully embrace and manifest WONCA’s mission both at home and abroad.
The WONCA mission is: …To improve the quality of life of the peoples of the world through defining and promoting its values, including respect for universal human rights and including gender equity, and by fostering high standards of care in general practice/family medicine. That mission can serve as a roadmap for our specialty so that we share the same goals and keep striving to improve people’s quality of life in an equitable and holistic way. It is relevant today just as it was in 1972. The concept of health care equity was soon after echoed for the wider arena of primary health care, in the Declaration of Alma Ata of 1978, which proposed five ideals as the foundation of all primary health care systems:
By definition as ideals , these concepts are somewhat idealistic. Moreover, they need much political motivation, capacity planning, infrastructure building, mobilisation of appropriately trained personnel,deployment of sufficient funds, and so on, in order to be realised. Thirty years later,in 2008,yet more recommendations were issued, this time by the World Health Organisation. Its World Health Report, titled “Primary Health Care: Now More Than Ever” re-emphasised the revolutionary societal role and impact that primary health care delivery could have, and it identified four key requirements for achieving co-ordinated and equitable person-centered care:
Importantly, these broad and deep principles involve and affect eve ryone in the community, and they introduce the concepts that health needs to be person-centered, needs to adapt to evolving expectations , and is essentially a human right .Nevertheless, those recommendations have been again very challenging to implement.
Fortunately, world leaders , stakeholders , educational and research institutions, and grassroots alike, have been motivated to redouble efforts and be held accountable for moving closer to sustainable health equity, through the eight United Nations Millennium Development Goals. The ambitious goals aimed for equity in health access, affordability, delivery, and outcomes. Their successful progress in 2015 have now led to 17 proposed Sustainable Development Goals, with a special focus on developing countries. Several of these goals are relevant to health, but number 3 is the most relevant to health care provision, preventive strategies, and health care resource planning in the next 10 to 15 years. Goal 3 is to ensure healthy lives and promote well-being for all at all ages. For some of the subgoals, Family Physicians can have a direct role. These include ensuring safe and healthy pregnancies and births, so as to reduce the global maternal mortality ratio and prevent infant deaths - although this does not seem to be relevant in Hong Kong as Family Doctors are rarely involved in maternal care and deliveries. Family Doctors, however, can help end epidemics and noncommunicable diseases through vigilance and patient education. We can help prevent and treat substance abuse in the community, and we can enhance sexual and reproductive care for both men and women. Some subgoals especially need creative thinking, political motivation and investment of human and financial capital worldwide, including in Hong Kong and mainland China, so as to achieve universal health coverage, innovation in drug development, long-term planning, and managing health risks.
Altogether, these goals encompass a wide variety of issues, including service delivery, public health, social care, health insurance, improving healthy lifestyles, training, resource planning, disaster preparedness, and policy making. This is the “bigger picture” of the global plan for solidarity and quality primary health care for the road ahead. The HongKong Academy of Medicine has had a great opportunity to make a difference and demonstrate leadership to help reach these objectives, such as through the Hong Kong Jockey Club Disaster Preparedness and Response Institute, which we hosted at our premises. Such advanced training helps Academy members and health professionals in Asia keep pace with emerging global trends in patient care and medical education. The Academy can also enhance global alliances, strengthen partnerships with institutions worldwide, and provide the most up-to-date training for our own future specialist leaders. But how can we, as Family Physicians, fit into the bigger picture, and how can we contribute to sustainable societal development? This is neither a minor issue nor a simple jigsaw-piece scenario. Actually, we can make, and it is our duty to make, a huge humanitarian contribution and difference to the local and global community, because we are uniquely placed at the frontline of continuous and lifelong patient-facing health services. Our aim is to deliver consistent, comprehensive, and continuous care for an individual in the context of the whole family and the community. We have to know all about all body systems and how to provide appropriate and sensitive care from cradle to grave. Therefore, what has been emerging in the past few decades is the realisation that the forefront of primary care, in fact, needs to be largely provided by Family Physicians.
A global discussion is thus gaining momentum about the growing importance of Family Medicine in primary care and how this fits into the overall primary health care delivery. On the one hand, family doctors need to work well with other primary health care providers, including other specialists, emergency services, paramedical staff and nurses, physiotherapists, community and social workers, public health workers, and so on. On the other hand, governments are earnestly formulating the best ways of achieving health care equity and universal coverage, with the associated issue of affordable and fair health insurance and subsidy. In Hong Kong, primary care development has been boosted by the founding of our College, a Department of Family Medicine and Primary Care at the University of Hong Kong, and the Primary Care Office in the Hong Kong Department of Health. Recent government media campaigns have been attempting to promote the image of the family doctor as a friendly extended member of the family who knows all family members and stays with the family as it grows, ages and develops. This image hopefully will help instill the 21st century habit of regular primary care visits to promote:
This gentle, voluntary strategy to encourage attitudinal and behavioural change is different from the tactic used in countries like Norway and the United Kingdom, where citizens register with a local family doctor or General Practition as their first point of contact with their national health service for nonemergencies. One of the aims of the Hong Kong method, hand-in-hand with innovative and equitable insurance reform, is to relieve the chronic pressure from the few low cost government primary care clinics and to discourage the use of emergency room services for nonemergencies. However, I have to say that the present Voluntary Health Insurance proposal under public consultation may actually have an opposite, knockon effect of reinforcing inappropriate health-seeking behaviour and creating more demand for hospitalisation. This would represent a huge step backwards from promoting care by Family Physicians at the community level. There must be appropriate amendments.
As we know, in-grained habits are hard to modify by external top-down policies. The motivation has to originate from within, after consideration of perceived benefit versus burden. Sometimes, ignorance is the reason for inaction, but today’s patients are becoming more and more media and technology-savvy. Still, they may put too much stock into sometimes dubious, inaccurate, and misleading online medical information. And they often also have an initial stance of “What’s in it for me?”, viewing preventive medicine to be too much hassle. They may prefer the traditional practice of seeking secondary and curative health care rather than primary and preventive health care. Or they may continue resorting to emergency services after ignoring and waiting until a problem really does become an emergency. Or they may self-medicate directly by going to the local pharmacy or traditional Chinese medicine shop.
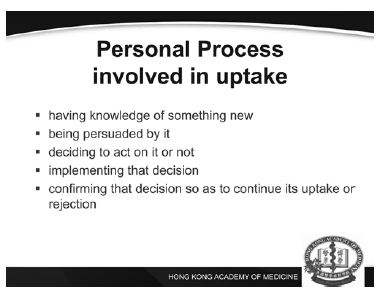
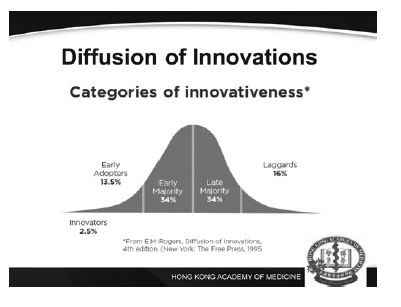
When patients do manage to visit a family doctor, instead of viewing the doctor as a caring long-term health partner, they tend to either treat the medical consultation merely as a service, demanding unnecessary drugs such as antibiotics and sometimes not even for themselves but for someone else. Or, they tend to treat the physician with complete deference, thereby deflecting responsibility for self-care to a wise know-it-all expert figure. Replacing these with the preferred scenario of a sustainable, equitable partnership to promote a preventive and life-long approach to primary care and health maintenance is, for some, a major paradigm shift. And yes, it does take a concerted effort and much energy from both sides. Think of the progressively different population sectors when it comes to their gradual acceptance, uptake, and use of a new technology, idea, or discovery as it spreads throughout a culture. According to Everett Rogers, they consist of a few innovators, followed by the early adopters, the early majority, the late majority, and finally a few laggards. Moreover, the personal processes involved in uptake can be summarised in five steps: having knowledge of something new, being persuaded by it, deciding to act on it or not, implementing that decision, and confirming that decision, so as to continue its uptake or rejection. The last confirmation step is what may give rise to cognitive dissonance and, for example, buyer’s remorse or a change of mind after a so-called cooling-off period. The first step of any social change is of course awareness , which is why marketing and social marketing campaigns often consider major influences such as:
These, coupled with explaining logic and research evidence, should in theory create the needed driving force for social behaviour change. Nevertheless, sometimes it takes a massive and large-scale crisis for mobilisation, action, and both horizontal and vertical coordination. Think of the Ebola disease or SARS, which took massive outbreaks to trigger governments,organisations, communities, health care workers, and researchers to finally get actively involved.
Even when the necessary research evidence is available, there still needs to be research translation and knowledge brokerage steps to push for widespread application and coordinated policy change. Think of handwashing to improve hygiene and control infection: the benefits of handwashing were demonstrated in the mid-1800s but the first national handwashing guidelines appeared only in the 1980s in the United States. Sometimes, a pioneering person or group needs to think outside the box to make the application of research findings practical and feasible.
I was recently in Boston and was privileged to meet the author of the best seller "Be Mortal" Dr Atul Gawande. He is not only a famous medical writer, a surgeon, but also the director of Ariande Labs which specialises in research in quality of care. The mission of the Lab is to create scalable healthcare solutions that produce better care at the most critical moments in people’s lives, everywhere. I look forward to working with him in assessing outcomes of quality of care in a healthcare system with enhanced primary care through the practice of family medicine. The development of research ideas into usable products is then followed by marketing and public education , while avoiding misinformation and disinformation. Think of penicillin, which took more than 10 years after discovery to be produced as a drug for clinical use. Ironically, physicians now have to re-educate the public not to misuse and over-rely on antibiotics. But Family Physicians have a duty and are well-positioned to do just that in our daily work in the community. In fact, insurance policies should place Family Physicians as the initial point of contact or gatekeeper for advice, treatments, possible referrals to other specialists, or arrangements for special procedures. It makes sense logistically and economically that way, but it does add a great sense of responsibility to our specialty owing to being committed to offering all-encompassing care for all ages.
At the same time, unfortunately, respect and trust are not automatically granted by patients or by other stakeholders. Respect and trust need to be earned and actively maintained. To that end, Family Physicians depend on branding, knowledge exchange, and mutual understanding among all our stakeholders. We must show a united front to raise the profile of our profession and specialty among patients and in society generally. Our College, originally named the Hong Kong College of General Practitioners, was officially established in 1977 as our united voice; to define and maintain high standards of training and continuing education , competence , and conduct ; and to professionally support its now 1500 members. Ours is not an easy job. So, the moral support aspect is important to prevent burnout, boost confidence, nurture leadership skills, and offer mutual encouragement and inspiration so as to keep striving for excellence in Family Medicine. Raising our public profile involves increasing public awareness of our family and community role, while also helping practising Family Physicians to engage in research and epidemiological studies in Hong Kong in order to expand our evidence base. Continued research is necessary to guide policy and best practices, and help plan for the future. As a College, we must educate Hong Kong citizens on whom and when to contact for medical and health services for primary care, but we must also develop programmes to provide continuing care with the Hospital Authority after hospitalisation. Furthermore , we have continuously been introducing the concept of Family Medicine education towards specialists in other disciplines as well as general practitioners who have not undergone vocational training. As for gradually educating our patients during consultations, we would do well to consider their context and overall health, and to show empathy and sensitivity. For the past decade or so, the trend has been to move away from simply aiming for patient compliance to a doctor’s instructions, towards clear and comprehensible doctor-patient communication and active patient involvement. This two-way exchange should naturally lead to patient adherence to a health intervention that has been mutually agreed upon, with the view to long-term holistic health and efficacious self-care. This is the interpersonal side of personalised and patient-centred health care delivery,and, I believe, this type of consistent, continuous, and culture-conscious face-to-face interaction is critical to motivating long-term behaviour and attitudinal change in people’s lives. Responding to the global call for primary health care reform requires clinic-level and national-level solutions. Both are complex, even more so when we realise the interconnectedness of our global village and fast developing trends. These common trends include national and international macro-economics, climate change, sustainability in natural and human resources, social-networking, global mobility, emerging diseases, reduced antibiotic efficacy, emerging technologies in the genomics era, and demography such as population ageing. Concerning international connectedness, our advantage is that our College is associated with WONCA, which is keen to coordinate a global cost-effective response plan for primary health care that involves Family Physicians. I contributed to their guidebook titled “The Contribution of Family Medicine to Improving Health Systems”, whose second edition was published in 2013. I highly recommend it, since it comprehensively describes our discipline’s roadmap, starting with a rationale, setting a goal, foreseeing roadblocks, and getting ready for action. Ultimately, the solution to responsive and equitable health care is going to take place at the integrated community and family and individual levels. So, we need to customise flexible, local responses to suit each region and community. In the clinic, our personal knowledge of each patient and his or her medical and family history, and even attitude towards western medicine, are all relevant to the consultation, intervention, and outcome.
Friends, Members, and Fellows of our College: In closing, I urge you to be ambassadors and leaders in our unique, exciting, and ever-evolving specialty. Keep learning. Stay aware of and adapt to your environment. Stay resilient. And keep making a world of difference in your journey in Family Medicine.
I wish to pay tribute to 2 forefathers of family medicine dedicating this oration to them. Dr Henry Li my late father and Dr Peter CY Lee.
Donald KT Li, FHKAM (Family Medicine), FHKCFP, FRCGP, FRACGP
President, Hong Kong Academy of Medicine Correspondence to :Dr Donald KT Li, 10/F, HKAM Jockey Club Building, 99 Wong Chuk Hang Road, Aberdeen, Hong Kong SAR, China.. |
|