June 2012, Volume 34, No. 2 |
Update Article
|
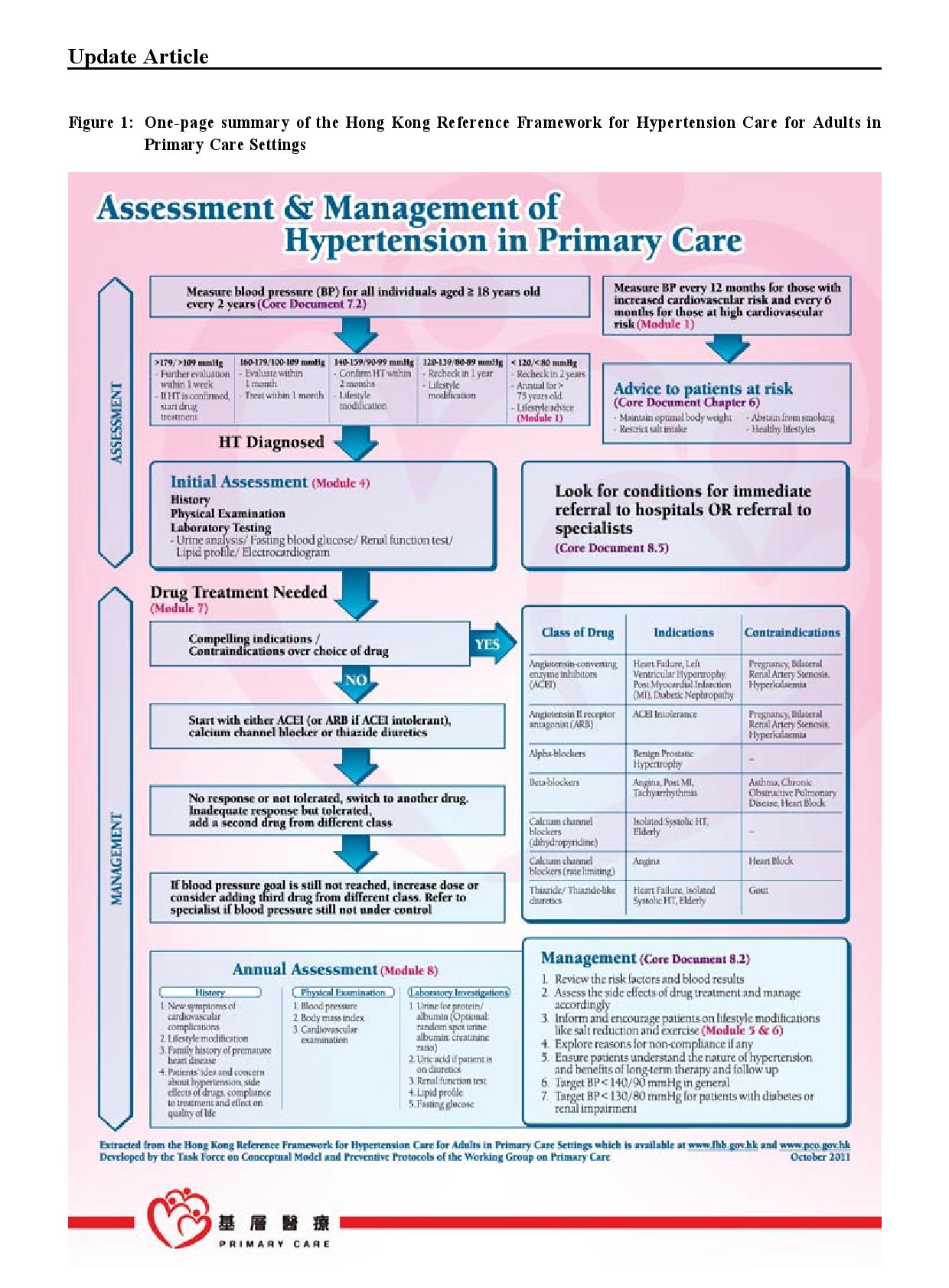
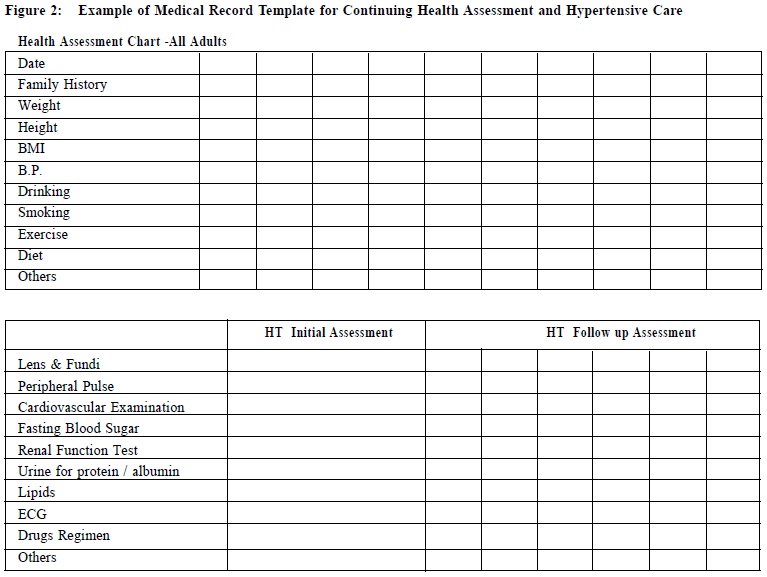
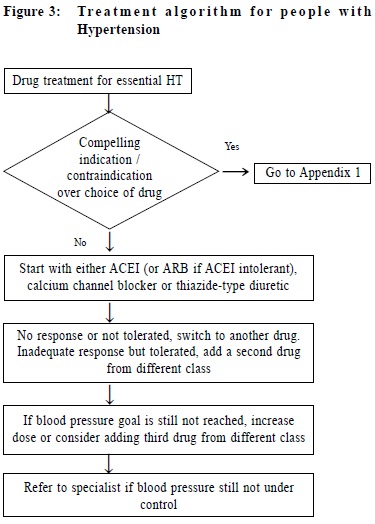
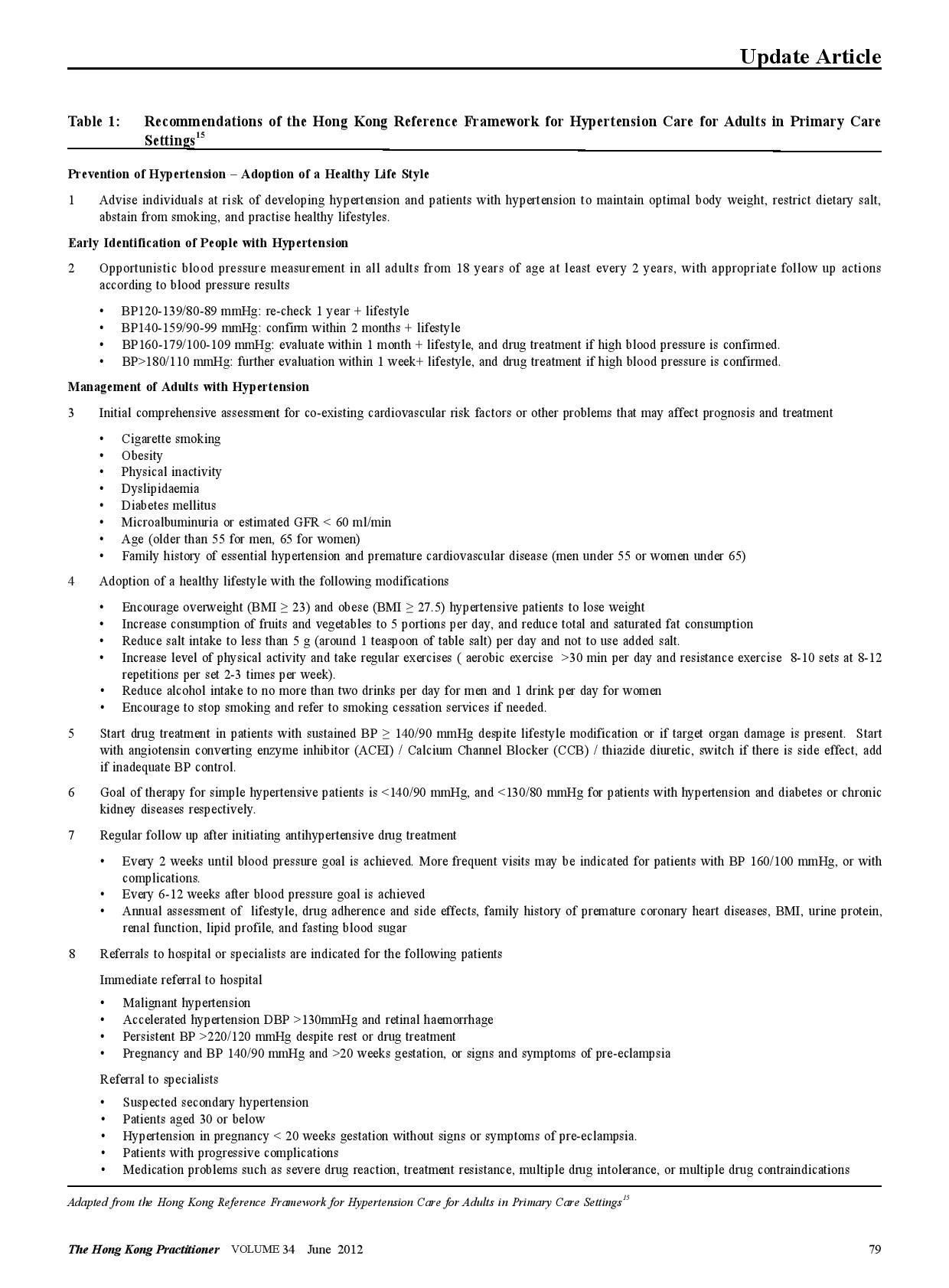
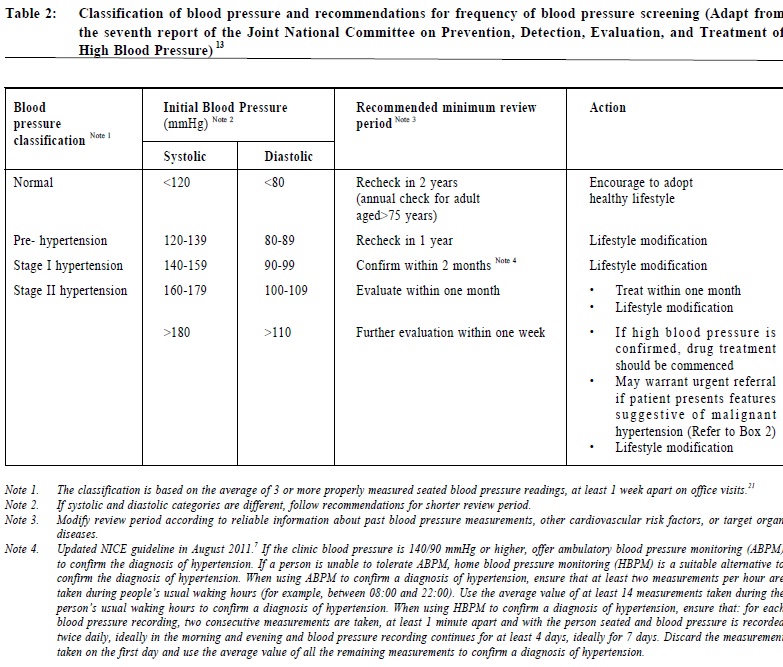
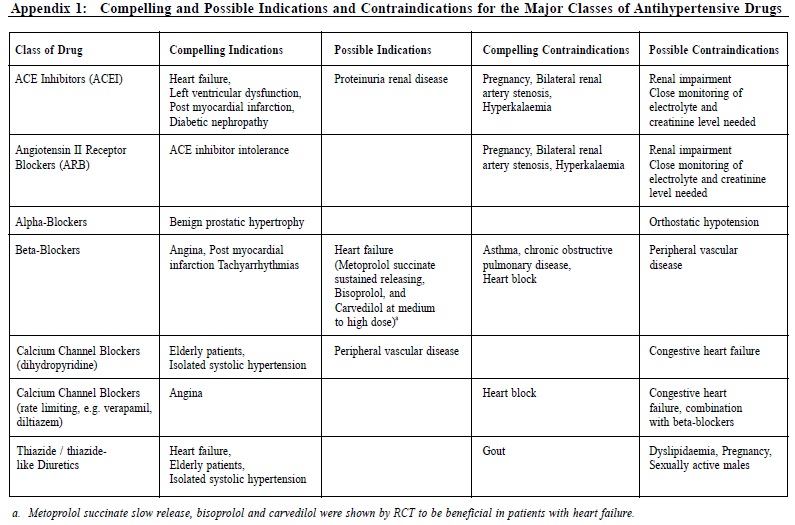
The Hong Kong Reference Framework for Hypertension Care for Adults in PrimaryCare Settings – translating evidence into practiceCindy LK Lam 林露娟, KH Ngai 魏家豪, Jeff PM Lee 李培文 HK Pract 2012;34:76-83 Summary Hypertension is the most common chronic disease among people aged 15 years or above in Hong Kong. It is the second commonest reason for consultation in primary care. The Reference Framework for Hypertension Care for Adults in Primary Care Settings was published by the Task Force on Conceptual Model and Preventive Protocols of the Working Group on Primary Care in 2010 in order to translate medical research evidence into health benefit of our population. It is a consensus document endorsed by various stakeholders including patient groups and primary care doctors and considered to be the most appropriate and feasible application of evidence to Hong Kong’s primary care. This article discusses how the family doctor can translate the Framework recommendations on hypertension management into daily practice. It is believed that adoption of the reference framework can lead to more effective management of this common chronic condition in primary care settings. 摘要 高血壓是15歲或以上香港人最常見的慢性疾病,也是基層醫療中的第二種最常見診症原因。為將醫學研究結果轉化成病人的健康效益,基層醫療概念模式和預防工作常規專責小組在2010年出版了治理成年人高血壓的參考概覽。這份文獻的制訂得到各方面人仕的共識,其中包括病人團體和基層醫療醫生的利益相關者。它被認為是在香港基層醫療最合適和可行的做法。本文論述家庭醫生可以如何將參考概覽中的建議應用在日常高血壓的預防及治療上。我們認為參考概覽的採用能在基層醫療更有效地處理這常見的慢性。 Introduction Hypertension is the commonest chronic disease in Hong Kong with a prevalence of 27% among people aged 15 years or above.1 It is the second commonest reason for consultation in primary care.2 The evidence on the association between high blood pressure and premature death and stroke has been known since the publication of the Society of Actuaries study on body build and blood pressure in 1959.3 Tens of thousands of research studies confirmed the harm of hypertension and the benefit of treatment to lower blood pressure. The Prospective Study Collaboration (PSC) meta-analysis of over a million subjects from 61 studies concluded that at all blood pressure levels down to 115/75 mmHg, a 10mmHg systolic blood pressure (SBP) or a 5mmHg diastolic blood pressure (DBP) reduction is associated with a 40% and 30% relative risk reduction (RRR) in stroke and other vascular mortalities respectively.4 Other studies have shown that a reduction of as little as 2 mmHg in DBP could reduce cardiovascular complications significantly.5 Many drugs have been shown to be effective in lowering blood pressure and reduction of cardiovascular complications.6,7 Translation of medical research evidence into health benefit of the population is always a challenge. Wilber and Barrow described the “rule of halves” in the rates of detection, treatment and control of hypertension were all around 50% among the relevant populations in the U.S. in 1972,8 which was later also observed in many other populations.9,10 The Hong Kong Population Health Survey 2003-2004 found that only 44.5% of those with high blood pressure were diagnosed.1 A survey on the management of hypertension among local primary care doctors found that only 30% would start treatment for patients with blood pressure >140/90 and the control targets of SBP < 140 and DBP < 90 were adopted by only 26% and 47% of the surveyed doctors respectively.11 To promote best practice, the World Health Organisation (WHO)12 and many overseas national professional bodies have developed guidelines on the treatment of hypertension.7, 13, 14 Similar initiative was also called for to assure the quality of care of hypertension for our population in Hong Kong.11 The Hong Kong Reference Framework The Hong Kong Reference Framework for Hypertension Care for Adults in Primary Care Settings, which is available online (www.fhb.gov.hk and www.pco.gov.hk),15 was first published in 2010 to address the needs of our local practice, and is being updated regularly. It is a consensus document endorsed by various stakeholders including patient groups and primary care doctors and is considered to be the most appropriate and feasible application of evidence to Hong Kong’s primary care. The framework consists of a core document and eight modules. Summary of the hypertension reference framework is shown in Figure 1. The core document describes the principles of the management of hypertension from primary prevention to patient empowerment for self-management, and makes evidence-based recommendations for practice as summarized in Table 1. Translating research evidence into daily practice The commitment of both public and private primary care doctors, to the prevention, detection and management of adults with hypertension is of primary importance. We need to assure the public that primary care doctors have the needed competence and support services to manage hypertension to a high standard. Prevention & Screening of Hypertension Every primary care consultation is an opportunity for preventing and screening hypertension. People in Hong Kong consult primary care an average of 8 times a year and 80% of the population would have consulted primary care at least once within a year16,17 which provides plenty of opportunities for doctors “to advise individuals at increased risk of developing hypertension and patients with hypertension to maintain optimal body weight, restrict dietary salt, abstain from smoking, and practise healthy lifestyles”, and to carry out opportunistic blood pressure measurement for all adults aged 18 or above.15 Classification of blood pressure and recommendations for frequency of blood pressure screening is summarized in Table 2.13 To ensure efficient service delivery to all eligible patients, a system for identifying eligible patients, accurate blood pressure measurement (Module 2 of Reference Framework), counseling on lifestyle modifications, recalling high-risk patients, and proper record keeping must be incorporated into routine practice. There should be an agreed protocol among primary care team members on who, when, what and how various tasks are to be carried out. The medical record must provide continuous recording and promote easy retrieval of blood pressure measurements as well as data on lifestyle, health advice, cardiovascular risk factors and other relevant parameters. An illustration of a supplementary record sheet or module for hypertension care is shown below (Figure 2). To serve the purpose, dietary and physical exercise advice needs to be very specific (Modules 5 and 6 of the Reference Framework).15 Repeated counseling and coordinated input from different health professionals including dieticians, physiotherapists (for exercise counseling), nurses from smoking cessation counseling clinic, are needed to enhance the effectiveness of various preventive advice.16, 18 It cannot be overemphasized that screening of hypertension is worthwhile only if patients with suboptimal BP are adequately reviewed in order to establish the diagnosis and to provide appropriate treatment. Hypertension should confirm if blood pressure is persistently high in at least 3 properly measured seated blood pressure readings, each at least 1 week apart during office visits. People with BP >180/110 mmHg should be further evaluated within 1 week; those with levels of 160-179/100-109 mmHg should be evaluated again within 1 month; while those with levels of 140-159/90-99 mmHg should be re-checked within 2 months to confirm the diagnosis, in addition to providing lifestyle advice (Table 1).15 Medical records of patients with raised blood pressure should be flagged for repeat blood pressure measurements. Furthermore the practice should set up a recall system to remind patients due for follow up. 24-hour ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM) for seven consecutive days are suitable alternatives for confirming the diagnosis of hypertension.7 A modeling study in the United Kingdom suggested that 24-hour ambulatory blood pressure may be the most cost-effective method for diagnosing hypertension19 but it needs to be confirmed by empirical clinical studies before it can be recommended as a routine practice. Management of Adults Hypertension Patients confirmed to have hypertension should be evaluated for possible secondary hypertension, coexisting cardiovascular risk factors, or target organ damage (Table 1). The details for evaluation on possible secondary hypertension and target organ damage assessment have been described in Module 3 and Module 4 of the Reference Framework respectively.15 To achieve this, direct access to reliable and affordable investigation services is essential. The treatment of hypertension starts with lifestyle modifications similar to those recommended for prevention, therefore support from relevant multidisciplinary services is necessary. Patients with malignant hypertension (DBP > 130 and heavy proteinuria, papilloedema or encephalopathy) or accelerated hypertension (DBP > 130mmHg and retinal hemorrhage) should be referred to the hospital immediately. Drug treatment should be started, if hypertension is confirmed, within one week for patients with blood pressure >180/110 mmHg, within one month for patients with blood pressure of 160-179/100-109 mmHg, and for those with sustained blood pressure of 140-159/90-99 mmHg despite lifestyle modifications for 6 months. Angiotensin converting enzyme inhibitors (ACEI ) , calcium channel blockers (CCB), and thiazide diuretics are recommended as first-line drugs for hypertension. Beta blockers are no longer recommended as first line drugs for uncomplicated hypertension. The choice of drug needs to be individualized according to other patient characteristics, e.g. diuretics should be avoided in patients with co-existing gout. A detailed description of the different anti-hypertensive drugs is described in Module 7 of the reference framework.15 Since some patients may be reluctant to commit to life-long anti-hypertensive drug treatment, continuing follow up and motivational counseling by the family doctor would be helpful. A treatment algorithm is illustrated in Figure 3. Patients should be followed up two weekly after initiation of drug treatment until the target blood pressure is attained, after which the follow-up intervals can be increased to 8-12 weeks. Over 90% of the adult patients with hypertension can be managed exclusively in primary care but referral to specialists for further management is recommended for patients with high risk of complications or features suggestive of secondary hypertension (Table 1). The family doctor Local research has shown that having a regular family doctor is associated with a higher likelihood of blood pressure screening and healthy lifestyle.20 The family doctor’s emphasis on a continuing trusting doctor-patient relationship and person-centred care is the key to the appropriate translation of recommendations into individualized management. However, family doctors are only part of the larger health care delivery system, the proper function of which requires the coordinated input from different partners including patients, the government, specialists, academia, other health professionals, laboratories, community services. The public and medical profession need to make a joint effort to prevent, detect and manage hypertension better in Hong Kong to break the “rule of halves”.8
Cindy LK Lam, MBBS (HK), MD (HK), FRCGP, FHKAM (Family Medicine) KH Ngai, MBBS (HK), FHKCFP, FRACGP, FHKAM (Family Medicine) Jeff PM Lee, MBChB (HK), FHKAM (Community Medicine) Correspondence to: Prof Cindy LK Lam, 3/F., 161 Main Street, Ap Lei Chau Clinic, Ap Lei Chau, Hong Kong SAR. References
|
|