|
June 2011, Volume 33, No. 2
|
Discussion Paper
|
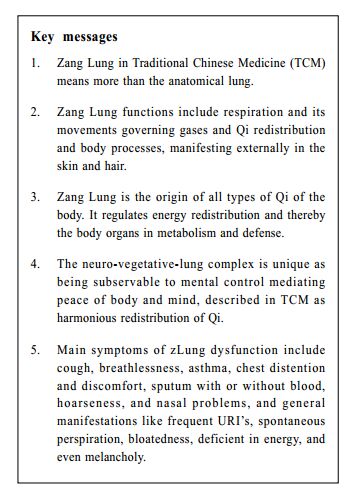
Understanding Traditional Chinese Medicine organs in the context of modern medicine – Part 4: Zang LungEdwin C L Yu 余秋良 HK Pract 2011;33:72-81 Summary This paper describes the organs of Traditional Chinese Medicine on a platform that they can be understood by workers in scientific medicine. The Zang Lung is discussed as the same anatomical organ but with added dimensions. Formalizing modern views from the Zangfu manifestation theory of Chinese medicine, it may embrace the whole respiratory tract and lungs, respiration functions, its associated cardio-circulatory effects, regulatory function on vegetative balance, defense resource utilization, and energy distribution mechanisms. 摘要 本文以現代醫學角度陳述中醫學的臟腑–肺臟。在此對中醫肺臟將以慣常了解的解剖學器官及其附加元素討論。按中醫學臟象理論,現代觀念中的肺臟可包括整個呼吸道及肺器官,呼吸功能,其有關的心肺推動力量,調節自在神經的功能,衞外的資源配套,及能量分佈的機能。 Introduction Zang organs 臟 in traditional Chinese medicine (TCM) depict solid organs which collect and store. Modern TCM workers tend to describe each Zang as a set of interrelated but remote parts rather than a single anatomical organ. To be more acceptable to modern medicine, my articles describe each Zang as one internal functional anatomical structure together with its external clinical manifestations.1-4 That perspective has been advanced by the belief that our ancestors started with essentially the same anatomical organ but with a wider dimension, and by using the platform expanded with an integral view additional to the usual mechanistic and functional view of current science. For most TCM starters, the Zang Lung may be the Zang that seems to be more easily depicted as equivalent to one anatomical organ. From a previous article, the Zang Spleen 1 is tied to two different functional anatomical parts, the splenic function and gastrointestinal function together, into one Zang organ structure. This is similar for zLung, which is paired internal-externally with, somehow oddly, the zLarge-Intestine. Thus, the perspective used in the last few articles would still be needed to help. The lung is the essential respiration organ to transport oxygen from the atmosphere into the bloodstream, and to release carbon dioxide from the bloodstream into the atmosphere. To reach the millions of thin-walled alveoli with specialized cells for exchange of gases, air passes through the mouth or nose, the larynx, the trachea, and a progressively subdividing system of bronchi and bronchioles. Healthy airway is maintained with bronchial secretion of immunoglobulin A, with production of mucus containing antimicrobial compounds like glycoproteins, mucins, lactoferrin, lysozyme and lactoperoxidase, and by the rhythmic upward beating action of the cilia to move up trapped dust particles and bacteria in the inhaled air. In addition to respiration, the lung also has non-respiratory functions including filtering out small blood clots and any gas micro-bubbles incidentally in the venous blood stream. The zLung is somehow different, TCM basically described the body in terms of functional entities. The Zangfu manifestation theory臟象學說expresses the Zang organs as organ networks by generalization from physiological and pathological manifestations of the body systems. Formalizing modern views from the theory, the zLung may embrace the whole respiratory tract and lungs, respiratory functions, its associated cardio-circulatory effects, regulatory function on vegetative balance, defense resource utilization, and energy distribution mechanisms. In short, Zang organs are different to the anatomical organs of the same name. Here, zLung is described as the lung with a wider dimension. Health care workers should appreciate these differences in terms and meaning since many patients use TCM and Western medicine both concurrently and interchangeably. Abbreviations of Zang Lung, Large Intestine, Zang organs are abbreviated as zLung, zLarge-Intestine, zOrgans described in previous papers. The zLung, Zang Lung
The lungs are located in the chest "on top of other viscera". The understanding
of zLung in TCM read 5 肺的生理功能是:主氣、司呼吸:通調水道:宣散衛 氣:朝百脉,主治節。肺在體合皮,其華在毛,開竅於鼻,在志為悲,在液為涕。手太陰肺經與手陽明大腸經相互絡屬於肺與大腸,故肺與大腸互為表裡。肺在五行屬金,在陰陽中屬陽中之陰,在人體氣和津液的代謝中是一個十分重要的內臟。
In short, the zLung includes not only the lungs, but also its pipes and vessels and the associated neurohumoral system. The functions of the zLung will be described separately under the respiratory system, when paired with the zLarge-Intestine, Qi utilization, and the regulatory function (Figures 1-4).
1. Respiratory system The body needs oxygen. The lung is responsible for this 肺者,氣之本. The lungs open through the nose. Clean air from the environment is drawn in and waste gas is exchanged out. A lot is described in Western Medicine. In general, while the zLung movements are inhalation and exhalation, its gas movements are described in TCM as dispersing (upwards, outwards) and descending宣降. This is then distributed throughout the body to maintain body tissues and organs. TCM emphasizes more on these respiratory movements and the tidal movement of gases. 1(a). Paired with zLarge-Intestine Justification of this internal-external pairing of zLung and zLarge-Intestine is a difficult problem to modern TCM workers. The ancient Nanjing saw it a problem as the large intestine and lungs are remotely placed.6 In fact, the transverse colon is separated from the lung just by the diaphragm and its attached subdiaphragmatic viscera. The large intestine is mainly involved with transport and transformation and functions to clear the unclean solid waste. Current TCM text tries to explain this pairing association by noting that the lung is the pushing power behind this action and large intestine blockages with constipation may interfere with the descending function of lung-Qi. In fact, the lung and abdomen may be seen as two compartments separated by the diaphragm in one enclosed ball, with the lung pumping with external air in the upper compartment and the large intestine in particular tuning the pump with internal gas and solids in the lower compartment. To support the body's strength, the lung of course is the important organ. How the thick abdomen is useful in strength can be seen in Japanese sumo wrestler. Also, constipated people tend to have a larger voice than those with a shallow abdomen. On the other hand, during Qigong training and exercise, in the early phase of body quality enhancement, there is increased gas passed per rectum, probably thereby increasing chest respiratory volumes. In general, the large intestine behaves as an up-down conduit 大腸接上傳下. The lungs help pushing the body waste material downwards all the way through the large intestine. People with constipation particularly use respiratory movements to push. The lungs help pushing the body waste material downwards all the way through the large intestine. People with constipation particularly use respiratory movements to push. 2. Qi redistribution In TCM, the word Qi (氣 air, gas) is used in a wider abstract ethereal context. TCM started its meaning from cosmic processes. In simplified terms, Qi has been referred to as physical or material energy. In the body, Qi can be classified into many types, but all bodily Qi has its physical origin in the zLung 諸氣者皆屬於肺. Qi in lungs includes air, lung-Qi and Zong-Qi 宗氣. Collective (Zong) Qi is the combination of Essence (Jing) Qi transformed from digested water and food with the lung-Qi. Zong-Qi accumulates in the chest, and then flows up to control respiration. Zong-Qi is the basic motive power of many physiological processes. The Zong-Qi in the chest, joining all vessels and channels 朝百脉, is distributed throughout the body to nourish the tissues and organs in maintaining the normal body functional activities. If the lung functions well, with even and harmonious inhaling and exhaling, there will be a related unobstructed circulation of Qi. Qi redistribution provides proper moisturization to the skin. Once the breath is regulated, the erratic processes of the body will calm down all by itself. If large intestine clearing process is in harmony with the zLung, the hair of the body and head will be lustrous. Similarly, the function of dispersion and descent would involve the distribution of Qi, blood, and body fluid to all the Zang-fu organs, the channel-collaterals, muscles, skin, and hair. The zLung also redistributes defensive Wei Qi to the body surface. Wei is the defence from nutrient fluid and granary of food 衛者,水谷之悍氣. Wei is coupled with Ying 營, the essence of assimilated nutrients in circulation, but moving beyond the circulation to traverse among tissues 營行脈中,衛行脈外, analogous to immune cells and chemicals. The dispersive action of the lung tidal waves delivers Wei Defence out the whole body and boundary peripheral tissues. The zLung functions to warm the tissues between the skin and muscles, replenish the skin, nourish the muscles, and regulate the opening and closing of the pores. Thus the zLung protects the organic body by defending against invasion of exogenous pathogenic factors. 3. Regulatory function The lung is situated atop the other organs. The two phases of zLung and lung-Qi movements include first, the out-clearing 宣發 with up-dispersive 升散 movements, and second, the orderly descending 肅降 movements. The balance of the two phases depends on the stability and dynamics of each phase. The two functions of dispersion and descent, while opposite to each other, act in unison for body regulation and maintenance. The zLung functions actively to expand downwards. In TCM, this characteristic is described as putting in order all descending movements within the body. By its pumping action, lending propulsive support from the heart, the lung functions in transporting essence to the other organs. The dominating drive on circulation is given by the heart by its high pressure wave down arteries to arterioles. A big breath lowers intra-thoracic pressure with increased venous returns and increased atrial blood volume. But the more significant contribution of the lung to perfusion would be the tidal pressure generated by deep breathing, flooding and emptying dynamically to perfuse tissues. This tidal perfusion at tissue level can be likened to a pump lubricating organs with essence. The lung is the only organ that the body can consciously alter its function, allowing it to have different dimensions of rhythm, depth and pace. By such manipulation, Chinese have developed breathing techniques to alter body physiology and balance. The lung up-down, expelling/in-sucking movements affect similar tidal movements in the tissues of the whole body. Besides denoting energy, Qi means processing and movements. TCM thus describes the zLung affecting the whole body Qi dispersive, up-down and tidal processes. Put in a wider perspective with the above characteristics, the zLung provides the tidal energy to the boundary and body border zones. Even and smooth respiratory cycles offer much to tissues and the body's peaceful balance. In other words, the phases of lung-Qi movement or their balance affect the Qi processes of the body. TCM describes the zLung as regulating the water passages 肺主行水. It means that the zLung supports water metabolism, regulates redistribution of water and excretion, and keeps the water passages clear. Its dispersing function circulates the nutrients assimilated from food and water throughout the body. Part of the fluid is discharged as sweat by the descending action of the zLung. Another part of the fluid is sent down to the kidneys and to the urinary bladder to be discharged. Thus the zLung is also known as the "upper source of fluid." Acclimatization and adaptive capacity The body changes and inteacts with the environment to achieve steady states of homeostasis. Taken aside the social and mental influences, the body adapts to and fits its surrounding physical environment. Acclimatization refers to the physiological adaptation to suit different conditions of climate or environment. A lot of studies have been done to address high altitude acclimatization. There are cardiovascular, respiratory and cellular metabolic changes to allow living in such a demanding environment. Andean and Tibetan, high-altitude natives,7 living in 60% hypobaric atmosphere, enhance oxygen acquisition with large lung volumes, the sum of vital capacity (VC) and residual volume. There will be more oxygen molecules per breath and a greater surface area for diffusion into the bloodstream. Tibetans have larger VC than Han Chinese long-time immigrants to Tibet. They maintain SaO2 (percentage of arterial hemoglobin saturated with oxygen) even during exercise while the immigrants cannot. Residual volume (volume after complete expiration) is doubled in these highlanders, allowing a larger oxygen store. The hypoxic ventilatory response or increase on exposure to hypoxia, which is not found after chronic hypoxic stress, is still maintained in Tibetan highlanders as a genetic trait and this adaptation is different from other highlanders. It is notable that, while acclimatization is perceived as a passive process, the body can actively acclimatize itself to its environment. Respiratory maneuvers are more easily actively addressed than manipulating the heart. Inhibitory impulses, produced by slowly adapting receptors (SARs) in the lungs during inflation, play a role in controlling typically autonomic functions such as breathing pattern, airway smooth muscle tone, systemic vascular resistance, and heart rate.8 "Pranayama" is the practice of voluntary breath control, and consists of conscious inhalation, retention and exhalation. The three phases can be either fast or slow. Pranayama is known to improve pulmonary function 9 and cardiovascular profile 10,11 with decreased heart rate and decreased blood pressure.12 Heat acclimatization can be facilitated with slow breathing. Pranayama has also been shown, over time, to reduce oxygen consumption per unit work 13 with increase hand grip strength.14 Pranayamic breathing with long breath retention could cause lowering of oxygen consumption and metabolic rate.15 Slow breathing over a period of three months was shown to improve autonomic function.16 Furthermore, slow pranayamic breathing, especially left nostril breathing, has been shown to increase volar galvanic skin resistance interpreted as a reduction in sympathetic nervous activity.17 For stress acclimatization, pranayama has been applied to autonomic nervous system imbalances,16 and psychological or stress related disorders.11,18 Breath holding has been shown to induce theta waves 19 indicative of parasympathetic activity. Decrease in breathing frequency would increase synchronization of brain waves eliciting delta wave activity 20 indicating parasympathetic dominance. These applications have been taken further in biofeedback programmes to vary and control other body functional modules. Poor stress acclimatization is often associated with rapid shallow breathing. Breathing with brief breath retention may cause significant increases in oxygen consumption and metabolic rate.15 Poor acclimatization may also be associated with increased intra-thoracic pressures. Pneumothorax has been attributed to fast breathing, Kapabhati breathing, in one case study.21 Intraocular pressure is generally decreased after aerobic exercise. Normal-tension glaucoma is more common in individuals who are subjected to frequent changes in eye pressure. Weightlifting may cause a temporary increase in pressure within the eye, with higher pressure particularly during breath-holding, and prolonged weightlifting could be a potential risk factor for the development or progression of glaucoma.22 Symptoms and signs of zLung dysfunction (Figures 1-4) The clinical manifestations of zLung diseases include those of the respiratory tract: cough, breathless, asthma, chest distention and discomfort, sputum with or without blood, hoarseness, and nasal problems. Other general manifestations include frequent upper respiratory tract infections (URIs), spontaneous perspiration, bloatedness, deficient in energy, and even melancholy. The zLung is known as the delicate organ. The lung has an innate aversion to cold, heat, dryness and dampness. It is also easily affected by nervous stress. When these delicate matters are upset, the zLung easily loses its clear and crisp equilibrium. Its rhythmic function may be deranged, and the free flowing Qi redistribution may become inefficient. The lung needs to be clear, conduit-smooth, unobstructed, unhampered so that the lung rhythm is balanced and effective. Affected by wind and cold, the nose will be congested. If the zLung is diseased, there may be frequent coughing. Symptoms of such upward Qi movement include a puffy face, an excessive desire to lie down, blemishes in the face, a yellowish pale-face colour, a cold nose, a headache, pain and distention in chest and back, restless extremities, itching of the skin, or obstruction in the throat. Lung diseases, chronic body diseases, exhaustion and stress cause a deficiency of lung-Qi. If lung-Qi movements fail to descend but instead ascends more, the disturbance may be manifested by stuffy chest, cough, asthma or emphysema. If there is a deficiency of lung-Qi, there will be feeble respiration, uneven breathing, weak speech and lassitude. If lung-Qi is deficient, the formation of Zong-Qi will be reduced. Then, not only gas exchange but also blood circulation will be disturbed and even obstructed, and then there will be chest distress, palpitation and blood stasis. The disturbance and weakness of the zLung function of promoting water metabolism may cause fluid retention and bloatedness. Severe pulmonary diseases and heart diseases are also related to each other. The modern TCM diagnostic criteria for lung-Qi deficiency should include at least three of the following: (1) weak and lethargic, (2) breathless and with lassitude to talk, (3) spontaneous perspiration, (4) bloated tongue with or without tooth-edged tongue, and, (5) weak pulse. If lung-Qi is weak and deficient, defensive Qi is not dispersed and the essential nutrients to the skin and hair are not distributed. On the one hand, this causes rough skin, dry hair, and spontaneous sweating. On the other hand, with deficient defensive Qi, the body is more vulnerable to attack by external pathogenic factors. Problems in zLung, especially when chronic, can affect the state of the zLung particularly its balance in Yin-yang and its dryness. The same may be caused by general diseases and illness of other organs. Yin-deficient zLung is noted by a red raw tongue. It may be associated with dry cough, small amount of sticky sputum, heat in afternoon or evening, night sweats, heat in the palms, dry mouth, dry itchy throat or hoarseness. Heat in zLung is associated with inflammation. Phlegm-fluids obstructing zLung is associated with ascites, pneumonia, and congestive heart failure. Reaction to wind affecting zLung includes URIs, with cold by wind for common cold and running nose, and heat by wind for flu and sore throat. Other illnesses related to zLung include the nose and the throat, the gateway of respiration, with dysfunction manifesting as stuffy nose, nasal discharge, dull olfaction, hoarseness of voice, and sore throat. Nasal mucus will be yellow and thick with heat or inflammation, pellucid and watery with cold, little mucus in production with dryness or with Yin-deficient zLung. Constipation may be due to a deficiency or stagnation of propelling power with inadequate Qi, or a general dryness related to the Yin-deficient zLung. Rectal prolapse may be due to various factors, but one cause is poor sphincteric tone related to inadequate Qi. In TCM, the feelings of sadness and melancholy are related to zLung. Excessive sadness and melancholy can impair lung-Qi and even cause the shortness of breath. The deficient lung-Qi with decreased Zong-Qi energy may cause feelings of sadness and melancholy. Confrontation with modern medicines The lung functions, breathing techniques, and biofeedback are not new to current medicine. Though their placement in some levels of good science may not meet the standards of critics, their use for those with body states tuned to their influences sometimes work wonders for improving energy, body functions, and psychosomatic illness including dermatitis. While there are many studies to define the effect of deep breathing on autonomous nervous system, studies on the more difficult delineation of its tidal effects at the tissue level are lacking. For those who find it difficult to appreciate or believe, try it on a morning in the days of tiredness or exhaustion. Stand snugly (not straight and rigid), breathe in deeply through the nose with loose jaws, hold breath briskly and then breathe out with jaws slightly eased forward after relaxing the tempero-mandibular joints. The thrust of fullness down through the trunk to the legs should be felt, resulting from the added tissue perfusion by that tidal respiratory wave on top of the on-going cardiovascular circulation. Thus while Western medicine had known much on gaseous exchange, there are still many areas worth deeper study. Yin deficiency and dryness of zLung are particularly notable since these are not observed in Western medicine. As URI symptoms are attributed to viral or bacterial infections, a sore throat would thus be taken as infection. But, loss of voice is observed after a day without sleep. A very sore throat with no signs of redness or swelling in the fauces is seen in an odd patient after two hotpots in hot summer. These should alert the skeptical physician to consider that there can be a change of the state of the mucous membrane not necessarily due to infection. TCM is particularly rich with medicine to irrigate the dry Yin-deficient respiratory membranes. Tuberculosis at the sick or late stages when body is weak or cachexic is highly associated with Yin-deficient zLung. Therapy on Yin deficiency significantly improved these body states and illness.23 Asthma on the other hand is associated with zKidney Yang deficiency and treatment on such would improve lung function and decrease relapse. On Qi-deficiency, breathing training was shown to improve symptoms and reduce bronchodilator use in asthma patients.24,25 The importance of understanding Qi-deficient zLung becomes more obvious with chronic emphysema when lung parenchyma and gaseous exchange is reduced to insufficient quota. Treatment of Qi deficiency in cardiopulmonary diseases is particularly helpful. TCM helps to improve paO2 and tissue oxygenation. Abstract words like Qi must be reduced to finer standardizable categories so that the herbal actions are not studied only with current standards. Until then, there will still be debatable conflicts between TCM and Western medicine around such issues. Conclusion The lung is well known to be central to the function of respiration. The TCM zLung description embraces its neuro-respiratory function with associated effects on the whole body. In Western medicine, the body systems were defined when it was once in a reductionist approach. The understanding and use of concepts of zLung allow us to see the whole body integral function in a broader perspective. The TCM body division into only five zang organs rather than many more organs may mean division of the lower brain functions into the five relevant characteristic neuro-autonomous functions associated with such major body organs. The zLung with its neuro-humoral set can be viewed as one department to face external energy demands and defence.
Edwin C L Yu, MRCP (UK), FRCP (Glasg), FHKAM (Medicine), RegCMP
Honorary Professor, School of Chinese Medicine, Hong Kong Baptist University.
References
|
|