|
December 2007, Volume 29, No. 12
|
Discussion Paper
|
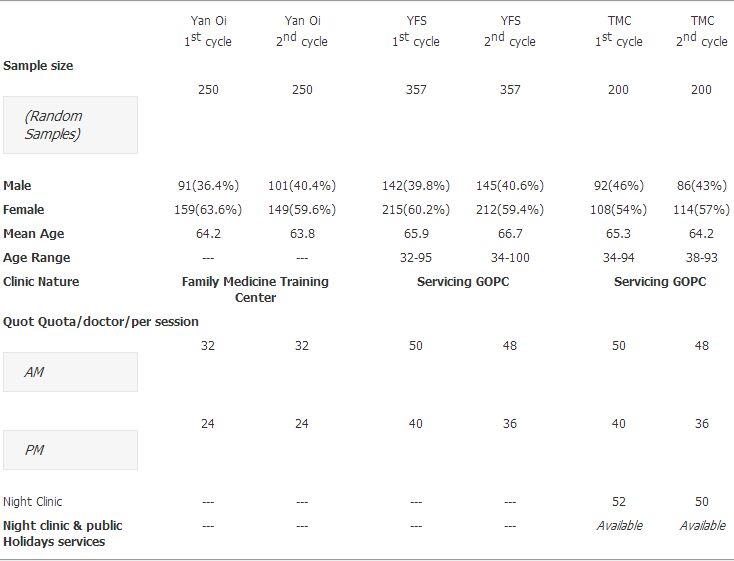
Management of hypertension in the General Out-patient clinics (GOPCs) of New Territories West Cluster: yesterday, today and tomorrowLaam Chan 陳嵐, Pun-nang Tsui 徐本能, Yeung-shing Ng 吳楊城, Chi-hung Chan 陳志雄, Hong-ning Suen 孫康寧, Dorothy To 杜潔玉, Jun Liang 梁峻, Cynthia S Y Chan 陳兆儀 HK Pract 2007;29:470-480 Summary This paper consolidated the results of three audits on hypertension care at the three General Out Patient Clinic in New Territories West Cluster over the period 2004 to 2006. Common baseline deficiencies identified in phase 1 of the audit cycles were: inadequate annual complication screening for end organ damage, cardiovascular risks assessments, lifestyle control, advice on non drug therapy and blood pressure control. Quality assurance strategies implemented were described. These included improving physicians' knowledge on hypertension management guidelines, improving record keeping by establishing individual patient record, specific attention to clinic structure and workflow logistics, involvement of the whole team at all staff levels and improving continuity of care. Computerized records greatly facilitated the carrying out of audits. Phase 2 audits showed marked improvement in the process of care. The proportion of patients with good blood pressure control rose by about 20% in each clinic. 摘要 本文綜合分析了新界西聯網其中3間普通科門診,由2004年至2006年度的3份高血壓管理質量審核報告。 審核的第一期發現每年併發症普查,心血管風險評估,生活習慣改變,非藥物性治療和血壓控制方面都有不足之處。 文章也 描述了所實施質量控制策略的具體內容,包括提升醫生對高血壓,特別是高血壓治療指引的知識。 加強病歷管理,建立個人化病歷。也特別留意以改善診療的流程及全體職員共同參與,以提升服務水平。 電腦化紀錄也有助於提高診所服務質量。第二期審核結果証實高血壓治療有明顯改善。每間診所的血壓控制良好率提升了20%。 Introduction In New Territories West Cluster (NTWC), the number of hypertensive patients increased substantially over the past few years with more than 60,000 hypertensive patients in December 2006.1 This paper aims to review the standard of hypertensive care, areas of deficiencies, quality assurance strategies implemented over the past three years, and the results and current standard achieved in the GOPCs of NTWC. The progress made was reflected in the major findings of three hypertension audits carried out in three individual GOPCs over the period 2004 to 2006. Size of the problem Hypertension is a common chronic illness and is the leading cause of mortality both in developed and developing countries.2,8 The prevalence of hypertension is increasing worldwide. New Orleans and Oxford researchers estimated that the overall prevalence worldwide increased from 26.4% in 2000 to 29.2% by 2,025. The absolute burden of hypertension was projected to increase from 972 million adult patients in 2,000 to 1.56 billion patients by 2,025, a 60% rise of total hypertensive patients.3 The relationship between blood pressure and risk of cardiovascular diseases was shown to be in a continuum and not confined to a subset of population with particularly high levels of blood pressure. Treating hypertension has been associated with about 40% reduction in the risk of stroke and about 15% reduction in the risk of myocardial infarction.8 Hypertension control was however unsatisfactory despite publication of many international guidelines.12,21,27-29,33-35 Globally, 29% of hypertensive in the United States, 17% in Canada, and less than 10% in European countries24,26 had their blood pressure under controlled. Locally, control rate was not more than 50%.4,23 Management of hypertension is still a challenge both globally and locally. There is a gap between daily practice and knowledge or evidence. In Hong Kong, essential hypertension accounted for 7,212 admissions to hospitals and 196 deaths at the year 2004/2005.5 In the community, it was the second most common condition seen in outpatient clinics after upper respiratory tract infection from two morbidity surveys 10 years ago.6,7 In New Territories West Cluster (NTWC), with increasing number of patients referred from hospital to community care, and patients being referred from private to government clinics for financial reasons, uncomplicated hypertension outnumbered upper respiratory tract infection to become the commonest condition seen according to our clinic statistics from 2004 to 2006.1 Historical background All together there were 7 GOPCs in NTWC namely Yan Oi, Wu Hong, Tuen Mun Clinic, Madam Yung Fung Shee, Yuen Long Jockey Club, Tin Shui Wai and Kam Tin GOPC. Yan Oi GOPC was first transferred from the Department of Health to Hospital Authority in December 2001. The rest were transferred to the Hospital Authority in July 2003. Scope of service and clinic hours remained the same before and after the transferal. Number of chits, total number of patients and consultation time allowed per case (except Yan Oi GOPC) were roughly the same (~50 to 52 cases per doctor in am session and 40 cases per doctor in pm session) but major adjustments in night clinic sessions (from 80 to 50 cases per doctor) was made. Yan Oi GOPC, being the community based training centre, had longer consultation time per patient to facilitate training. What was in our past? On the whole, the standard of hypertensive care in terms of process performances and blood pressure control was found to be unsatisfactory in 2003 in all 7 GOPCs. Three hypertension audits were done in three GOPCs by three different doctors over the period 2004 to 2006. All three audits included random samples of uncomplicated hypertensive cases (K86 of ICPC coding) only. Complicated hypertensive cases, pregnancy induced hypertension, secondary hypertension and those who were not regular attendants of that particular clinic were excluded. Most of the studied criteria were similar among the three audits aiming to assess the process performances and outcome of blood pressure control. They however had different focus and emphasis because of different clinics settings and needs. The standards set for each criteria were different among the three audits because the individual author had different justifications. Reasons for the justifications would not be elaborated in this paper (details please refer to individual audit reports9-11). Criteria and standard of each audit were attached in Table 1, 2 and 3. From 2004 to 2005, an audit of uncomplicated and isolated hypertensive cases (without diabetes) was carried out in the Yan Oi GOPC. ICPC coding for uncomplicated hypertension (K86) occupied about 25% of the total ICPC counts in 2004 from the clinical management system(CMS).1 Since December 2001, the clinic was transferred to the Hospital Authority and converted into a family medicine training centre. Shortly after the transfer, a group of doctors in the clinic developed management guidelines for hypertension which was based on 1999 WHO/ISH Hypertension Guidelines. The quality of care given since the guidelines were set up had not been evaluated. Thus an audit aimed to evaluate the process and outcome of hypertension management in Yan Oi was carried out. Audit criteria (Table 1) were set based on international guidelines,12,13 Eli Lilly Clinical Audit Centre14 and Department of Health (HKSAR) Hypertension Working Group.15 Among the 250 random samples in first cycle in 2004, only blood pressure readings (97.2%), smoking status (96.4%), diabetes (98.4%) and cholesterol (84.8%) assessment were satisfactorily documented. However, the performances of drug compliance documentation (58%),non-pharmacological advice (38.4%), annual assessment of urine for albumin (14%) and body mass index (14.4%), physical inactivity (42.4%) and family history (3.6%) assessment were far below the guideline standards. 47.2% of patients achieved satisfactory blood pressure control in the first cycle. (Table 1) From 2005 to 2006, an audit on uncomplicated hypertension management in the Madam Yung Fung Shee GOPC which was a busy and traditional GOPC providing day time clinic service, was carried out. ICPC coding for uncomplicated hypertension (K86) occupied 27% of total ICPC counts from CMS in 2005.1 357 patients were randomly selected out of 5,401 uncomplicated hypertensive patients in the 2005 first cycle. The audit protocol (Table 2) was adopted and modified from the Eli Lily National Clinical Audit Centre and standards updated based on evidence-based international guidelines. Results of first cycle in 2005 showed that hypertension registry, pretreatment blood pressure levels and referral of refractory cases to hospital specialties standards were met. All other criteria were far below standard. (Table 2) From 2004 to 2006, a clinical audit on uncomplicated and isolated hypertension (without diabetes) in Tuen Mun Clinic was carried out. This clinic was also a traditional busy GOPC. Apart from day session, it also provided services at night clinic sessions and public holidays. Uncomplicated hypertension was the commonest condition seen in Tuen Mun Clinic since 2004. ICPC coding for uncomplicated hypertension (K86) occupied 30% of total ICPC counts in 2004. The audit protocol and criteria were set to focus on those weakest areas observed in Tuen Mun Clinic. (Details please refer to Table 3). 200 out of 4,756 random samples were selected in first cycle in 2004. Results of first cycle showed that all the studied criteria were below standard except for diastolic blood pressure control. The performances were worse for the night clinic cases in the sub-analysis of day and night clinic results. (Table 4) Characteristics of the three clinics, patients" demographic data and profile were summarized in the following table:
Major areas of deficiencies identified a) Clinic factors Unsatisfactory quality of medical records, busy clinic with limited consultation time and lack of alert or reminder system were the main issues. b) Staff factors For doctors, time constrain was the major difficulty. It was easier to repeat drug regimen than to review the drug regimen and adjust accordingly. Doctors usually focused on blood pressure readings alone but overlooked other important parts including revision of diagnosis, correctness of coding, lifestyle modification in particular for those at risk, record of body mass index (BMI) and body weight (BW) monitoring which were the essential part of the routine management process. Other areas of inadequacies included annual complication screening, non drug management, on-going cardiovascular risk assessment, assessing drug compliance and adverse drug effects with proper documentations. Lack of standardization on entry of clinical parameters such as BP readings, BW, BMI and adverse drug effect were also observed. c) Patient factors About half were elderly patients older than 65 years of age. Education delivery would be technically very difficult, especially for those with hearing or visual impairment. Underprivileged, lower social class and lack of insight of our patients made them less ready to accept health advice. d) Problems specific to night clinic sessions Difficulties to ensure continuity of care as all patients were on walk-in basis. Number of nursing staff was less during night clinic sessions. Routine complication assessment or health education was not available. Doctors" performance might decline at the end of a whole day's work (from 9 am to 10 pm). What had been done over the past three years? Major strategies implemented in all GOPCs of NTWC were: a) A good medical record became mandatory for good clinical care
b) Adjustment of the number of quota per doctor per session at night clinics Quota was reduced from 80 to 52 per doctor session. The total number seen each night was maintained by increasing the number of doctors on duty. The number of patients per doctor was further reduced from 52 to 50 after the implementation of the computerized records in night clinics. c) Revision and update of knowledge regarding evidence based guidelines and recommendations on hypertension management to colleagues at department seminars
d) Streamlining the workflow of the clinic for hypertension visits
e) Beginning of Nurse Led Clinic in GOPC This was run by Advance Practice Nurse (APN). Elderly patients confused about drug regimen or non-compliant patients with poor BP control were referred to the APN for individual health education on chronic disease knowledge, lifestyle modification and monitoring of diet and drug compliance. f) Improved continuity of care and appointment booking for chronic cases
g) At individual clinic levels There were orientation programmes for new doctors about the roles and requirement expected. There were increased teaching and communication between the doctors and the nursing and supporting staff. The annual complication checklists were designed and adopted at individual clinics to improve standard of care. h) Patient education
How is it today? All three audits showed significant improvements on second cycle data collection after a period of 12 to 18 months intervention: a) In Yan Oi Clinic Poorly performed criteria in the first cycle, namely drug compliance, advice on non drug therapy, urine protein, body mass index, and family history of coronary heart disease had statistically significant improvement in the second cycle. Among these, only blood pressure documentation, smoking status, diabetes and cholesterol assessments reached the standards. (Table 1) b) In Madam Yung Fung Shee Clinic There was statistically significant improvement for all criteria except criteria 1 (hypertension registry) and criteria 8 (refractory hypertension/possible secondary causes being referred to specialties) as they were already very good (performance = 100 %) in the first cycle. Among these, accuracy of new case diagnosis, follow up intervals, annual fasting blood and lipid profile assessment and blood pressure control for non diabetes met the set standards. (Table 2) c) In Tuen Mun Clinic There were major improvements in most of the criteria being studied in the second cycle. Those achieved statistically significant results included exercise advice from 11.5% to 25.5%, BW/BMI measurement from 10.5% to 38.5%, renal complication screening from 35.5% to 80.5%, cardiovascular complication screening from 30% to 60.5%, cardiovascular risks assessments from 35.5% to 75.5%, assessment of drug compliance from 68.5% to 91%, assessment of drug adverse effect from 13% to 57.5%, and satisfactory systolic blood pressure control from 60.5% to 82%. The improvements were even greater in night clinic sessions. (Table 3 and Table 4) In summary, major improvements seen consistently in all three audits included lifestyle assessment, advices on non drug therapy, annual complication screening for end organ damage, cardiovascular risks assessments, and blood pressure control. (Table 5) Limitations
Discussion Other than updating the knowledge of doctors on hypertension diagnosis and management, all the practical implementation strategies and protocols were important for the better process outcomes, attention to the details of coding, data entry, workflow of clinic, clarification of roles of the doctor, nurse, supporting staff, appointment booking and/or recall of defaulters, initiation of annual screening protocol, etc, were essential. Communication among all members of the team and ongoing discussion with feedback of results were also important for the audit's success. Positive use of audits was improvement of all team members from grass root level, with goal of better patient care rather than a punitive approach of fault finding. Sharing of the results of improvement will generate more enthusiasm to adhere to guidelines. Medical records and computerization, with the ability to quickly retrieve data for audit and feedback are essential tools for chronic disease management. Prompting and decision support features to facilitate guideline adherence will enhance the capacity of the electric medical record. Continuity of care, preferably by the same doctor, is shown to improve our quality of care for chronic illnesses. Though this may be technically difficult (roster shift for training or service needs) for institutions, we tried to explore ways to achieve this as much as possible. Evidence kept changing and regular updating is needed because what we regard as correct now may be wrong tomorrow. During the time of the 2nd cycle data collection in September 2006, there was an update in the NICE and BHS guideline on hypertension16. Beta blockers were no longer recommended as the first line treatment for hypertension based on evidence from 20 clinical trials particularly the Anglo- Scandinavian Cardiac Outcomes Trials (ASCOT).17 The evidence suggested that beta blockers performed less well than other drugs, specifically in the elderly, and more evidence indicated that beta blockers at usual doses carried an unacceptable risk for provoking Type 2 diabetes mellitus. Though we had significant improvements in the second cycle, only a few criteria were able to meet the standard set by each individual clinic. Do we still have room to make further progress? Or are we already stretched too much given the limited resources, i.e. the consultation time? This is the question of idealism versus realism. The consultation time has remained largely the same over past 10 years (~5 minutes per case) but the disease pattern has changed. Hypertension outnumbered upper respiratory tract infection become the commonest condition seen in GOPCs. Furthermore, all these quality assurance processes, namely computerization record, proper data entry, coding, patient education, complication screening challenge doctors" consultation time. Extra time may be needed to manage patients with other chronic illnesses, emotional disorders, or more complex physical problem. We need to rationalize our expectations within the limited resources. If further progress is expected, further input of resources including manpower, reasonable consultation time and training need to be considered, as well as more patient education and health promotion, e.g. teaching and facilitating patients to monitor their own BP at home, improving accessibility of home BP monitors, practical diet and exercise adherence programmes. Conclusion With the increasing number of hypertensive patients and hypertension being the commonest condition seen in GOPCs, primary care doctors are responsible to update his/her knowledge regularly, and must be able to apply the knowledge into daily practice to provide a high standard of care. GOPCs of NTWC have undergone a series of quality assurance strategies over the past three years and achieved a significant improvement on hypertensive care as evidenced by the results of three hypertension audits done in three GOPCs. Major improvements consistently seen in all three audits include lifestyle assessment, advices on non drug therapy, annual complication screening for end organ damage, cardiovascular risks assessments and better blood pressure control. There is still room for further improvement as many of the standards had not been met during the second cycles. What is the way forward? Reinforcing patient education and improving public awareness on hypertension should be emphasized. We are looking forward to maintaining our service standard, to continue the quality assurance strategies and to continue the audit spirals to sustain the improvements and further progress over a reasonable time interval and ultimately to reduce the long term morbidities and mortalities of hypertension. Whether we can "control" the hypertension "burden" tomorrow, depends greatly on how well our standard of patient care is today. Acknowledgement We cannot implement any quality assurance exercise without the support from our department heads. On the other hand, any quality assurance strategy will not be successfully carried out without the actual work of front-line staff. So, our achievements belong to every member of the department. Whether we can sustain our achievements or not depends largely on whether we can uphold our team spirit and team morale. We would also like to express our thanks to and acknowledge the contributions of all front-line medical staff, nursing staff, health care assistants, supporting staff and clerks for their hard work and cooperation to achieve the above improvements in the busy GOPCs. Special thanks to Dr Au SY and the Hospital Authority Family Medicine Coordinating Committee for directing and supporting quality improvement policies and electronic cord system. Key messages
Laam Chan, MBChB, DFM(CUHK), FRACGP/FHKCFP
Medical Officer, Pun-nang Tsui, FHKAM (FM) Medical Officer, Yeung-shing Ng, BMedSc (CUHK), PDip Com Geri (HKU), PDipCAH (HK), FHKAM(FM) Medical Officer, Chi-hung Chan, MBBS (HK), DFM (CUHK), PDip Com Geri (CUHK) Senior Medical Officer, Tuen Mun Clinic GOPC. Hong-ning Suen, MBBS(HK) Senior Medical Officer, Madam Yung Fung Shee GOPC. Dorothy To, MBBS, FRACGP, FHKCFP, FHKAM (FM) Senior Medical Officer, Jun Liang, FHKAM(FM), MRCGP(UK) Consultant, Cynthia S Y Chan, LMCHK, MD (Canada), FHKAM (FM), FRACGP LMCHK, MD (Canada), FHKAM (FM), FRACGP, Department of Family Medicine, NTWC. Correspondence to : Dr Chan Laam, Department of Family Medicine, Tuen Mun Hospital, N.T. Hong Kong.
References
|
|