|
July 2003, Volume 25, No. 7
|
Update Articles
|
||||||||||||||||
Management of vulvovaginitis in childhoodS S C Chan 陳丞智, G W Y Cheung 張惠恩, P M Yuen 阮邦武, R K H Chin 陳健浩 HK Pract 2003;25:319-324 Summary Vulvovaginitis is the commonest gynaecological problem in premenarchal girls. Patients usually present with pruritus vulva, pain, vulval redness, vaginal discharge or bleeding. The most common cause is non-specific vulvovaginitis. General advice in perineal hygiene and voiding habits will help most patients. Other less common causes are infection, systemic illness and occasionally child abuse. Recurrent or persistent symptoms require referral to paediatric gynaecology unit for thorough gynaecological assessment and further management. 摘要 外陰陰道炎是女性外陰和陰道的炎症,是尚未經歷初潮的少女最常見的婦科問題。 病人通常表現為外陰瘙癢、發紅,有陰道分泌物甚至出血。最常見的病因是非特異性外陰陰道炎; 注意會陰部衛生和良好的排泄習慣等一般建議對多數病人都有作用。 其他較少見的病因有感染、全身性疾病,偶而也可能是兒童受到虐待所致。 症狀反覆發作或遷延不愈的病人應轉給兒婦科醫生,以便進行徹底婦科檢查和進一步治療。 Introduction Vulvovaginitis is inflammation of the vulva and vagina in response to various stimuli. It is the commonest gynaecological problem in premenarchal girls. Although the actual incidence is unknown,1 it is not uncommonly encountered in general practice.2 Risk factors The genitalia of the prepubertal child is less well protected than that of a woman of reproductive age. The vaginal mucosa is thickened at birth from prenatal oestrogen stimulation. Thereafter and before menarche, the vaginal mucosa is thin and atrophic because of the lack of oestrogen, making it more susceptible to irritation and infection. The vaginal orifice in children is less well protected by the underdeveloped labia. It is close to the anus, and the risk of faecal contamination is high. All these factors together with a tendency of poor hygiene in small children add to the risk of vulvovaginitis. Most vulvovaginitis in childhood are non-specific, but a minority is associated with infection, systemic illness and occasionally child abuse. History Childhood vulvovaginitis usually presents with pruritis vulva, redness, pain and vaginal discharge. Some patients may have vaginal bleeding (Table 1).1,3,4 Abdominal pain and dysuria with or without frequency occur in 26% and 51% of children.3
The colour and nature of the discharge can help to differentiate between physiological discharge and bacterial infection. Foul-smelling discharge may result from a foreign body. Urinary symptoms, enuresis and constipation should be considered. Other aspects of the child's history should be elicited, for example, the toileting, perineal hygiene, habits of bubble baths or use of deodorant soaps, other medical illness including diabetes mellitus and dermatological disease. A history of recent upper respiratory tract or skin infections of the child or family member may suggest secondary -haemolytic streptococcal vaginitis. Behavioural changes, nightmares, fears, headaches and enuresis should raise the possibility of sexual abuse. Typically, the parent or caregivers will give the history. However, the child should also be included, as this may help to establish a rapport. Information of bathing, perineal hygiene, and placement of anything into her vagina can be asked. She may also be asked to demonstrate her motion of wiping or scratching. Examination The approach to examination depends on the age and comfort level of the child. The child should never be forced to have an examination of her genitalia and instruments should be avoided. Adequate communication, constant reassurance and repeated explanation of the examination steps to the child and her parents are crucial to the success of examination. Using slang and words used in their homes will help. A running conversation about toys, cartoons and school often diverts the child's attention and helps her cooperate with the examination. It is also helpful to show the parent the examination findings. If the child is unable to cooperate, the examination should be deferred. The examination usually involves an inspection of the vulva, anus and or lower vagina. The anus and vulva should always be examined for cleanliness, excoriations, erythema, discharge, blood, trauma or other lesions. Then the vagina should be visualised. However, examination of the vagina may not be essential if the cause of the vulvovaginitis is confirmed by inspection of the external genitalia. The knee-chest position or the supine position with the child's legs flexed on her abdomen enhances visualisation of the genitalia. In the knee-chest position, as the child takes deep breaths, the vaginal orifice falls open. As the vagina is short in prepubertal girls, the presence of foreign body or lesion in the vagina can often be diagnosed using this approach.5 The rectal examination is important in girls with persistent discharge, vaginal bleeding, or pelvic or abdominal pain. It allows the palpation of hard foreign bodies or abnormal masses in the vagina and helps to express vaginal discharge not previously seen. The examination should be performed gently using the little finger. If vaginal discharge is present during the examination, samples should be obtained for culture. Special care should be taken to avoid touching the hymenal edge, as this will cause discomfort and pain. Causes The aetiology of vulvovaginitis in childhood is different as compared with adolescents and adults. Physiological leucorrhoea may be one of the causes. Among 50 premenarchal girls over 2 years of age who presented with redness, soreness or itching of genital area with or without genital bleeding, 80% of them had no evidence of infection.1 Patients with an infectious cause usually present with more significant discharge and redness of the genital area. Fewer than 5% of patients have vaginitis caused by sexually transmitted diseases. Poor perineal hygiene is also considered as an important cause of vulvovaginitis in children.1,3,6
The maternal oestrogen passed in utero to the foetus can cause mucous secretion by the endocervical glands. The discharge is characteristically white, mucoid and without odour. It is not associated with vulvovaginal inflammation. This physiological discharge persists for a few days. In some babies, the discharge may contain blood owing to the withdrawal of maternal oestrogen and the resulting endometrial shedding. After the newborn period, there is no more visible vaginal discharge. During puberty, in response to the increase in oestrogen level, physiological leucorrhoea begins. A whitish mucoid discharge may start weeks to months before menarche and may continue for several years. As the menstrual cycle becomes more regular, the girl may notice a cyclic variation in vaginal secretions associating with the cyclical changes of the oestrogen and progesterone levels. There is copious watery secretion at midcycle and stickier and scantier discharge in the second half of the cycle. In Hong Kong, there is a lack of health education to the adolescent to provide information about puberty, menarche and change in vaginal secretions. Reassurance and explanation to the patient is the only treatment required. The mother may also apply her own experience onto the child, thus explanation to the mother or caregivers is also required. Non-specific vulvovaginitis accounts for the majority of childhood vulvovaginitis, ranging from between 25-93% in various series. The pathogenesis and associated alteration in vaginal flora have not been well defined. Some organisms are part of the normal vaginal flora. These include Staphylococcus epidermidis,1,7 enterococci and E. coli1,7 and Diphtheroids.1 The predominant anaerobic bacteria are Peptococcus and Peptostreptococcus, Veillonella parvula, Eubacterium, Propionibacterium and Bacteroides.7 Lactobacilli are however less common. Despite normal flora, vulval irritation may develop because of poor perineal hygiene, or special irritants such as tight-fitting clothes, nylon underpants or stockings. Once inflammation occurs, scratching may follow, and superimposed bacterial infection may occur. Treatment is usually directed towards improved hygiene, avoidance of irritation, and techniques to promote the dryness of the vulva. Routinely prescribing antibiotics should be discouraged. General measures for nonspecific vulvovaginitis include the following:
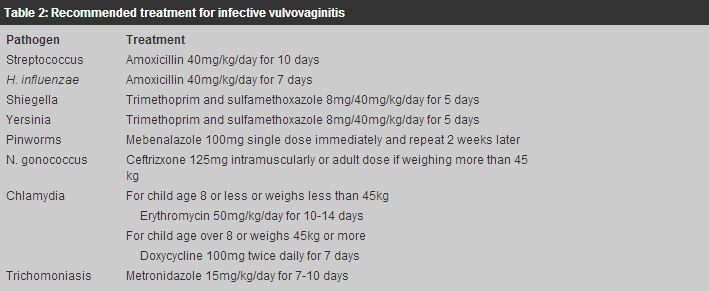
When vulvovaginitis is persistent, an infective cause, foreign body and sexual abuse have to be considered. The child should be referred to a paediatric gynaecology unit for assessment and management. When vaginal discharge is seen during examination, it should be obtained for culture to identify the pathogen. These are often respiratory, enteric, or sexually transmitted pathogens. The treatment is summarised in Table 2.
Respiratory pathogens of vulvovaginitis in children include group A
Group A
The significance of Haemophilus influenzae as a pathogen for vulvovaginitis remains debatable. It is commonly isolated in children suffering from vulvovaginitis.3 However, it was also found in 5% of normal girls.9 If Haemophilus influenzae is the only pathogen identified in a symptomatic girl, a trial of oral amoxicillin is indicated. Shiegella is an enteric pathogen that can spread from the gastrointestional tract to the genital region in prepubertal girls. The typical presentation is mucopurulent and sometimes bloody vaginal discharge. The treatment is trimethoprim and sulfamethoxazole. Yersinia enterocolitica has also been identified as a cause. The treatment is also trimethoprim and sulfamethoxazole. Candida is a rare cause of vulvovaginitis in children. Treatment with topical antifungal agent such as nystatin, miconazole, or clotrimazole applying to the external vulva is recommended. If symptoms persist, intravaginal antifungal cream or pessary in suitable size will be required. Pinworm infestation by Enterobius vermicularis is a frequent problem in young children. The typical symptom is perianal and vulval itchiness at night. The diagnosis can be made if parents can see the worms at night. A morning "Scotch Tape" test can also identify the eggs at the perianal region. The treatment is oral mebendazole. Sexually acquired vulvovaginal infections in prepubertal child include those caused by Neisseria gonorrhoea, Chlamydia trachomatis, Trichomonas, herpes simplex and human papillomavirus. Gonococcal infection usually causes a greenish purulent, mucoid vaginal discharge. The child may also complain of dysuria and pruritus vulva. Chlamydia trachomatis in the vagina of infants can be due to perinatal maternal-infant transmission, which may persist for over a year. However, in prepubertal girls, it is associated with sexual abuse. Because of this implications, the diagnosis should always be made by cell culture. Trichomoniasis rarely occurs in prepubertal girls because the unestrogenised vagina is relatively resistant to the infection. It can also be transmitted from mother to child during childbirth. Both type 1 and 2 herpes simplex viruses can cause vulvovaginitis in prepubertal children. This can be spread by oral infection or be a consequence of sexual abuse. The diagnosis should be considered when there are typical ulcers and vesicles. It is followed by culture confirmation. Human papillomaviruses can be transmitted by perinatal exposure, sexual abuse or close physical contact. Genital warts presenting before 2 years of age are generally acquired perinatally. As the age of the child increases, there is increasing suspicion of sexual abuse. It is a challenge to detect sexual abuse as many children do not disclose their abuse. Physical findings are often absent or nonspecific. Physical indicators may include pain, burning sensation, irritation in the uro-genito-anal area, vaginal discharge, genito-anal bleeding, recurrent vaginal infections, and abdominal pain. The isolation of a sexually transmitted organism may be the first indication that abuse has occurred. Any child detected to have the sexually transmitted pathogen should be considered victim of sexual abuse. Sexual interaction with peers, toys or animals, enuresis, sleep disturbance may be other indicators. The incidence and prevalence of sexual abuse of children are difficult to estimate, mainly because many escape detection. According to a questionnaire survey of 2,147 Hong Kong Chinese college students, the overall prevalence was 6%, and the rate was higher in females than males.10 Only 39% of the victims reported their sexual victimisation to others, and 56% of the reported incidents were not followed up. Although the study showed a lower rate of child sexual abuse in Hong Kong as compared to Western countries, constant alertness and a high index of suspicion is still needed. Once suspected or diagnosed of sexual abuse, the victim should be referred for specialist's care, for proper assessment and diagnosis, ruling out sexually transmitted disease, providing social and psychological care and legal advice. Their siblings too should be screened for sexual abuse. A vaginal foreign body should be considered if the discharge is persistent, bloodstained or foul smelling, especially if there is no identifiable pathogen and the discharge or inflammation fails to respond to treatment. The most common foreign object is a balled-up wad of toilet paper. When foreign body is suspected, visualisation of the vagina can be done using labial traction method or knee-chest position. The rectal examination can also allow palpation of hard foreign bodies. Vaginal lavage using warm saline or water can remove the fragments of toilet paper in a cooperative child. Topical lidocaine gel applied to the hymen can reduce pain from the procedure. However, for a heavy object or the foreign body being embedded in the vaginal epithelium, or in an anxious child or reluctant parent, the child will require examination under anaesthesia. Vulval dermatitis is a frequent cause of vulvitis without vaginitis. The vulva may be affected by seborrheic dermatitis, psoriasis or eczema. Viral infections such as varicella, measles and rubella, and systemic diseases such as leukaemia, erythema multiforme, Crohn's disease, and Kawasaki's disease are rare causes of childhood vulvovaginitis. Conclusion Vulvovaginitis is not an uncommon condition in general practice. The most common aetiology is non-specific vulvovaginitis. General advice on perineal hygiene and voiding habits will help most patients. Antibiotics are only required in infective vulvovaginitis. Children with persistent or recurrent symptoms, vaginal bleeding and suspected sexual abuse are best referred to a paediatric gynaecology unit for detail assessment and management. Key messages
S S C Chan, MRCOG
Medical Officer, G W Y Cheung, MRCOG, FHKAM(O&G) Medical Officer, P M Yuen, MRCOG, FHKAM(O&G), FHKCOG Consultant, R K H Chin, FHKAM(O&G), FRCOG, FHKCOG Consultant, Department of Obstetrics and Gynaecology, New Territories East Cluster, The Chinese University of Hong Kong. Correspondence to : Dr S S C Chan, Department of Obstetrics and Gynaecology, Prince of Wales Hospital, Shatin, NT, Hong Kong.
References
|
|||||||||||||||||