|
July 2003, Volume 25, No. 7
|
Update Articles
|
Health maintenance for the elderlyR S Y Lee, K W Kwong 鄺家驊, K S Ho 何健生 HK Pract 2003;25:307-318 Summary The number of persons aged 65 and above has increased dramatically in Hong Kong. Comprehensive physical, functional, social and psychological assessments including the use of simple and easily administered assessment tools to identify specific problems that are common in the elderly, followed by health education and holistic interventions can provide effective primary care health maintenance for them. 摘要 香港六十五歲及以上人口迅速增長,全面的身心及社交生活綜合評估,附與簡易評估工具可以及早發現長者常見的問題,再配合相應的健康教育及全面治療,便能為長者提供有效的基層醫療保健。 Introduction Hong Kong has achieved one of the world's best health indices. Life expectancy has risen from 72 to78 years in male and 78 to 84 years in female and the age-standardised death rate has dropped from 5.6 to 3.3 per 100,000 standard population from 1981 to 2001. The longer life expectancy and lower mortality rates contributed to our ageing population. The population aged over 65 has risen from 6.6% to 12% of our total population from 1981 to 2001. It is projected that by 2031, 24% of our total population will be over 65.1 Non-communicable diseases (e.g. cancer, stroke, diabetes and heart diseases), injuries, and neuropsychiatric conditions are major health burdens.2 The incidence is increasing especially among our elderly population. In Hong Kong 75% of those aged 65 or over suffer from one or more chronic diseases.3 The leading causes of death are malignant neoplasm (33.0%), heart diseases (16.3%) and cerebrovascular disease (10.5%).4 Suffering from chronic diseases causes loss of physical and mental capacity, which in turn leads to functional disability and dependency with considerable economic implications. Identifying these diseases and their risk factors, with modifications of individual lifestyles and environmental influences, can prevent or even reverse these situations. Older people are more prone to accident-related injuries such as falls and paedestrian/traffic accidents. Injuries cause enormous functional and psychosocial disability even though they may not be a major cause of death. In 1997, there were 127,305 patient-days due to fractured neck of femur in Hospital Authority hospitals in Hong Kong, ranking fifth among all diseases. Prevention of injury therefore is important for older persons, and the WHO policy framework for active ageing in 2002 has declared fall prevention as one of the important issues to be addressed. Neuropsychiatric conditions that are particularly related to elderly persons are depression and dementia. In Hong Kong, the suicide rate among those aged 60 or above was 29.6 per 100,000 as compared to the all ages suicide rate of 11.9 per 100,000.1 Screening to identify depressed patients in primary care settings and appropriate treatment decreases clinical morbidity.5 With the concept of ageing-in-place for old people and their special demands on medical and social resources, primary care physicians need to provide a holistic approach for care of the elderly. An annual physical check up alone may not cater for all their needs. Comprehensive assessments on the physical, psychological, social and functional needs, unique to the older population, should be adopted. Using simple and easily administered assessment tools, physicians can improve identification of specific problems that are common in the elderly. The focus should shift from disease-specific intervention to preventive care and proactive medical intervention. Prevention of cardiovascular and cerebrovascular diseases Coronary heart disease and stroke rank number two and three as the leading causes of death in Hong Kong. The two accounted for 16.3% and 10.5% of all deaths respectively in 2000.1,4 These conditions have a predilection for the elderly population resulting in significant disabilities and becoming a health burden to the society. Every effort should be made in order to combat their major risk factors such as smoking, lacking of physical activity, obesity, hypertension, diabetes mellitus and hyperlipidaemia.
Advocating a healthy lifestyle including smoking cessation, promotion of regular exercise, optimisation of body weight and low fat diet advice should be made at every opportunity. Behavioural modification needs time, knowledge, patience and good doctor-patient rapport. The advantage of repeated interactions with patients and trustful relationships developed over time gives family physicians much opportunity to educate and motivate our patients to change. The benefits of exercise have been well documented.6 Exercise decreases mortality and age-related morbidity through cardiovascular training, muscle strength improvements, balance and increase flexibility. The practice of "Tai-chi-chuen" is an effective exercise in improving balance and preventing falls among the elderly.7 The Canadian Task Force on Preventive Health Care remarked that there was insufficient evidence to recommend for or against community based obesity prevention programmes because weight reduction methods are of limited long-term effectiveness. However, because of the considerable health risks associated with obesity, prevention of obesity should be a high priority of health care providers.8 For obese adults with obesity-related diseases (e.g. diabetes mellitus, hypertension), weight reduction is recommended. Smoking is responsible for up to 30-35% of myocardial infarctions9 and is a major contributor to stroke.10 In elderly Chinese patients, smoking is a risk factor for many disease mortalities, as well as fatal and non-fatal stroke.11 Stopping smoking results in reduced cardiovascular mortality within one year.12 Smoking is a major cause of death in older Chinese men and quitting smoking saves lives.13 Stopping smoking as early as possible is important, but cessation at old age also provides meaningful life extensions. There is good evidence to screen and to treat hypertension.14 Blood pressure checking is the single most important activity in reducing morbidity and mortality in the elderly because of the significance of vascular diseases and the proven effectiveness of hypertension treatment in improving outcomes. Systematic review of the literature from the Cochrane Collaboration showed the benefit of detecting and treating systolic and diastolic hypertension in individuals between the ages of 60 and 80.15 Several large, randomised placebo-controlled trials that included persons aged 60 years or over demonstrated that anti-hypertensive treatment in elderly persons significantly reduced mortality from all causes by 12%, stroke by 36%, and coronary heart disease by 25%, as well as stroke and coronary heart disease morbidity.16 The positive effect of reducing high blood pressure in the elderly is actually greater than it is in younger persons.17 Excellent evidence is available to support screening and treating hypercholesterolaemia in those with known coronary disease. However, serum cholesterol screening for the elderly for primary prevention is still a controversial issue. Recent studies such as the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER)18 and the Heart Protection Study (HPS)19 have demonstrated that cholesterol-lowering therapy effectively reduces coronary and total mortality rate in high-risk patients, and the highest incidence of coronary heart disease occurs in persons aged 65 or over. Thus, the recent US Preventive Service Task Force (USPSTF-3) guideline sets no upper age limit for cholesterol measurement. The prevalence of non-insulin dependent diabetes mellitus increases steadily with advancing age. It is found that 14.1% of community-dwelling elderly population in Hong Kong has diabetes.4 Routine screening for diabetes mellitus in asymptomatic adults is still debatable. The American Diabetes Association (ADA) recommends screening for diabetes all individuals having risk factors, including obesity, family history, history of glycosuria during pregnancy and a few selected medical conditions.20 The WHO also concluded that opportunistic screening of high risk persons may be beneficial to permit earlier intervention.21 The cancers Cancers have been the leading cause of death in Hong Kong since the 1960's, claiming one in every three deaths in year 2000. The common sites of cancer are lung, liver, colon, stomach, and rectum in descending order and accounted for 60.2% of all cancer deaths.4 Recommendations about cancer screening differ substantially among various authorities. Cancer screening decisions require weighing quantitative information, such as risk of cancer death and likelihood of beneficial and adverse screening outcomes, as well as qualitative factors, such as individual patient's values and preferences. In general, patients with life expectancies of less than 5 years are unlikely to derive any survival benefit from cancer screening.22
Cervical cancer remains an important cause of morbidity and mortality in the elderly, predominantly in those without a prior history of adequate screening.28 Those who have not been screened in the past (including many women currently older than 65) are more likely than younger women to have abnormal smears or invasive disease. In fact, it is found that 25% of invasive cervical cancers occur in women older than 65. Although no absolute evidence, performing several Pap smears before ceasing screening seems prudent and reasonable in women older than 65 unless there is a clear history of regular previous screenings in which the smears have been consistently normal.
Breast cancer is responsible for 3.5% of all cancer deaths in Hong Kong in 2000.4
Report published in the past year have contributed to rising doubt about the value
of breast cancer screening. The USPSTF reviewed 8 trials and found a non-significant
trend towards decreased breast cancer mortality in screened younger women (age range
40-49) and a significant reduction in older women (age
Routine clinical breast examination alone or breast self examination has not been found to reduce mortality from breast cancer. In their 2001 report, the Canadian Task Force on Preventive Health Care recommends against teaching breast self-examination to women aged 40-69.27 Colorectal cancer ranks number three as a major cause of all cancer deaths in Hong Kong in 2000.1,4 Colon cancer screening has been controversial, but consensus has emerged in the last few years. Digital rectal examination is not effective as a screening tool for rectal cancer. For asymptomatic people at normal risk, there is good evidence that it is beneficial to initiate annual or biennial faecal occult blood testing (FOBT) starting from age 50 and above.29,30 However, it is necessary to screen 10,000 persons for 10 years to prevent 8.5 deaths. Periodic sigmoidoscopy and colonoscopy have also been shown to be effective in reducing mortality in colorectal cancer. However they are expensive, not readily available, with risk of complications, and often uncomfortable to patients. They are probably best reserved for persons at higher-than-normal risk, such as those with strong family history of colon cancer in first-degree relatives or of familial polyposis. Lung cancer is the commonest cancer death in the elderly, but screening with chest x-ray or sputum cytology is ineffective in reducing its mortality. Health education including smoking cessation is associated with reduced cancer risk even in long-term smokers. Screening asymptomatic elderly for other cancers (e.g. pancreatic, ovarian, uterine and testicular) is not recommended, because there is no evidence of its effectiveness. Fall prevention In a local study of elderly Chinese aged 70 and over, the rate of fall in the past 12 months was 32%.31 Falls are responsible for a significant number of deaths and injuries due to accidents among the elderly. More than 90 percent of hip fractures are associated with falls. Elderly persons who survive a fall experience longer hospital stay, faster functional decline and are at greater risk for subsequent institutionalisation. The psychological impact of a fall results in fear of falling and increasing self-restriction which often leads to dependence and increasing immobility.32 Risk assessment for falls includes a review of all likely intrinsic and extrinsic risk factors. Intrinsic factors include age-related physiologic changes such as postural control, gait, visual ability, diseases that affect sensory input, the central nervous system, musculoskeletal strength, coordination, and medications. Extrinsic factors are the environmental hazards such as poor lighting, slippery floor, obtrusive furniture and bathrooms with no grab bars or handrails. A single fall may have multiple causes, and repeated falls in an individual may warrant careful assessment of all the intrinsic factors.32 Some simple balance and gait tests have strong correlation with falls. One-leg balance test predicts injurious falls though not all falls.33 It is tested by having the patient stand unassisted on one leg for five seconds. The patient chooses which leg to stand on and balances himself. In the "Get Up and Go" test, the patient is observed and timed to rise from a sitting position, walk 10 feet, turn and return to the chair to sit.34 Taking more than 16 seconds suggests an increased risk of falling. Any observed or reported changes in gait, strength, or balance may require further evaluation. Measures to reduce risk of falls include elimination of environmental hazards, improving home supports, socialisation, modification of medication, balance training and regular exercises. The senses
Visual impairment is associated with decreased ability to perform activities of daily living and increased risk for emotional depression and falls. The Snellen eye chart can be used as a tool for visual acuity screening in the elderly. Visual impairment is defined as acuity of less than 20/60 in the better eye, with the best correction.35 The most common causes of visual impairment in the elderly include presbyopia, cataract, age-related macular degeneration (ARMD) and glaucoma. The prevalence of visual impairment is high, and under-reporting is common. 41.7% of attendants of elderly health centres of the Department of Health were found to have cataract.36 Both the USPSTF and Canadian Task Force on periodic health assessment recommend visual impairment screening for the elderly.37,38 Presbyopia is universal with ageing, and is readily corrected with eyeglasses but many old people may not be wearing appropriate corrective glasses. Appropriate correction resulted in 54% of subjects having improved vision by at least one line on the Snellen chart. Cataract causes progressive visual loss. Treatment with cataract removal and intra-ocular lens implantation improves vision, mental status, writing and fine-motor control. ARMD is a leading cause of blindness. Risk factors include hypermyopia, a family history of ARMD, smoking and chemical exposure at work. Distorted near-vision and blurred vision are the most frequent first symptoms. The presence of many drusens, pigmentary changes of "softening" may be detectable by ophthalmoscopy by primary care physicians. Laser photocoagulation can improve preservation of visual acuity in patients with ARMD and this offers a rationale for early detection and observation of ARMD.38 People aged 65 or above are at high risk for glaucoma. The earliest symptom of open-angle glaucoma is loss of peripheral vision, which frequently goes unnoticed. Methods to detect chronic open-angle glaucoma are tonometry, inspection of the optic disc and perimetry. The use of the Schitz tonometer in screening is not recommended due to its poor sensitivity and low positive predictive value.39 Other methods of measuring intra-ocular pressure (e.g. puff tonometry) are now available but their performance in community screening is still to be determined. Experienced family physicians are able to recognise an increased optic cup-disc ratio in excess of 60% of patients, with sensitivity and specificity both exceeding 90% for the diagnosis of glaucoma. Annual screening for diabetic retinopathy by fundoscopy with pupil dilatation or retinal photography is recommended for diabetic patients as treatment of proliferative retinopathy by photocoagulation is effective in preserving sight. Screening with retinal photography is slightly more effective than with fundoscopy using the ophthalmoscope.38 In a local study, 19.1% of patients attending the elderly health centres have hearing loss.36 Ninety percent of presbycusis is due to sensorineural hearing loss resulting from age-related changes. Hearing impairment can affect physical, emotional, cognitive, behavioural and social functioning and may lead to social isolation and depression. Hearing aids can improve the patients' quality of life. With its high prevalence and effective intervention, there is good reason to screen for hearing impairment among the elderly.40 Screening for hearing loss includes a questionnaire, physical tests and pure-tone audiometry. The question "Would you say that you have any difficulty hearing?" was found to have a 90% and 83% sensitivity, 71% and 75% specificity for detecting a 40dB hearing loss at 1000-2000Hz and 1000-4000Hz respectively in the two ears. The whispered-voice test, and finger-rub test were found to have sensitivity of 80-100% and 80%, specificity of 82-89% and 49% respectively. The audioscope can be used as a simplified audiometer which was found to be performing consistently with 87-96% sensitivity and 70-79% specificity.41 It allows inspection of the external auditory meatus and tympanic membrane, and using a standardised series of pure tones, gives considerable accuracy and inter-observer agreement in assessing hearing. Mental status
Reported prevalence of depression in the elderly population ranged from 0.8% for major depression to 26% for affective disorders and neurosis. Depression is the main psychological factor that results in the elderly person harbouring a suicidal wish or feeling that life is not meaningful. In Hong Kong, the suicide rates for those aged 65-74 and 75 or above were 27.7 and 48.8 per 100,000 respectively. This is high compared to 7.3 and 9.1 in UK, 11.8 and 16 in Australia, 17 and 13.6 in New Zealand, and 16.4 and 35 in selected urban areas of China.42 The USPSTF now recommends screening adults for depression in clinical practices that have systems in place to assure accurate diagnosis, effective treatment, and follow-up.43 The Geriatric Depression Scale (GDS) is a good screening tool to use in older patients. The Chinese version of the GDS had been validated as a screening instrument for depression among the Chinese elderly in Hong Kong with high sensitivity and specificity.44 An assessment for suicide risk is important in geriatric patients who appear depressed. Direct, yet non-threatening questions of whether they are concerned that they are becoming a burden to their family or whether they have ever felt that their family might be better off without them, followed by questions about active suicidal ideation, can be used. The prevalence of dementia increases with age, roughly doubling every 5 years. Dementia is easily recognised in its advanced stages, but clinicians fail to detect an estimated 21%-72% of patients with dementia, especially when the disease is early in its course. In a local community survey, 4% of those aged 65 or above, and 6% of those aged 70 or above suffered from dementia. The prevalence was 10.7%, 18.8% and 25.8% in those aged 80-84, 85-89 and 90 or above respectively.45 The most commonly used screening tool for dementia is the Mini-Mental State Examination (MMSE). It is valid, reproducible with 90% sensitivity and 80% specificity. There is a validated Cantonese version. Level of education and cultural differences have important effects on the range of MMSE scores in a given population. Applying a uniform MMSE cut-off point may miss significant changes among well-educated patients and generate false positive results among persons who are less educated or from different cultures. The Clock Test is another simple and quick test with 92% sensitivity and 97% specificity for the detection of moderate to severe dementia. Since it examines a lesser range of cognitive function, it is not as sensitive as the MMSE for detecting early dementia and is not useful as a screening test.46 The potential benefits of detecting dementia are identification and treatment of the reversible causes of dementia such as drug intoxication, depression and metabolic abnormalities, reducing morbidity associated with dementia, and preparing patients and their family members for problems that will arise as dementia progresses. However, Canadian Task Force on Preventive Health Care remarked that there was insufficient evidence to recommend for or against screening but physicians should be alert for any reports or behaviour which might indicate cognitive impairment, and then pursue appropriate strategies for further investigation and treatment.47 Urinary continence The Hong Kong Continence Society reported 18.1% of male and 36.6% of female aged 60-74 and 29.5% of male and 39.5% of female aged 75 or above suffered from urinary incontinence including stress incontinence. Incontinence causes significant social and emotional distress, hygienic problems, and places a burden on both patients and their care-givers. However, relatively few patients request treatment or volunteer that they are having problems. Straight-forward questions for screening urinary incontinence are "Do you ever lose urine when you don't want to?" and "Have you lost urine on at least six separate days?" Evidence of stress incontinence is elicited by the question "Do you ever lose urine when you cough, exercise, lift, sneeze or laugh?" Further assessment should include evaluation of cognitive function, fluid intake, mobility, medication side-effects and previous urologic surgeries. Physical examination should focus on the lower genitor-urinary tract in women and the prostate gland in men. A rectal examination can determine the presence of faecal impaction, and a simple urinalysis can screen for infection or glycosuria.48 Functional assessment One important aspect of healthy ageing is to be able to live independently. Periodic assessment on improvement or deterioration in functional ability gauges therapies of chronic illnesses which are not curable in a tangible and practical way. Besides, ability to function is prognostic of mortality49 and it also has practical value in advising and counselling patients and their families on the level of services needed to lead an independent living. Functional assessment comprises activities of daily living (ADL) and the instrumental activities of daily living (IADL). The ADL are functions fundamental to independent living such as bathing, dressing, toileting, transfer from bed or chair, continence and feeding. The IADL are more complex daily activities such as using the telephone, preparing meals, and managing money.
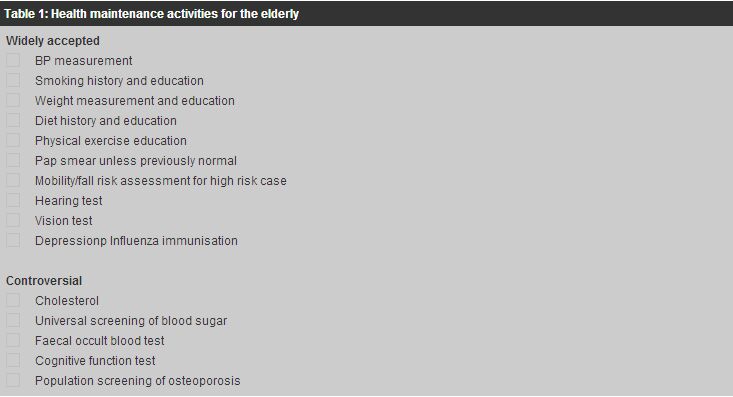
The Katz Index of ADL includes bathing, dressing, toileting, transfer, continence and feeding. A 3-tiered scale consists of the ratings "independent", "semi-independent" and "dependent" is found to be reliable and reproducible even by personnel with minimal training.50 The modified Barthel Index assesses the need for home health services by assessing the patient's ability for self care with items weighted for the amount of physical assistance required to carry out functions of feeding, bathing, grooming, dressing, toileting and transferring.51 A simple screening test of five items which are travelling, shopping, meal preparation, housework and handling money determines who may require a more comprehensive assessment.49 Regular screening in a primary care practice identifies areas of deficiencies and deterioration and this can translate readily into services needed. Conclusion With the special demands on available medical and social resources, systematic health assessment on various areas of potential geriatric risks can be performed, wherever opportunity arises or periodically, to develop a database appropriate to the unique concerns of elderly patients. In fact similar health maintenance programmes conducted by the Department of Health and some non-governmental organisations have been well received by the elderly. Using simple and easily administered assessment tools, physicians can improve the identification of specific problems that are common in the elderly. The focus of treatment should shift from disease-specific intervention to preventive care and proactive medical management in order to maintain maximal independence, function and quality of life.
Key messages
R S Y Lee, MBBS(HK), MPH(CUHK), Dip Derm(London), FHKAM(Family Medicine)
Senior Medical Officer, K W Kwong, MBBS(HK), P Dip Com Ger(HK), FHKAM(Family Medicine) Senior Medical Officer, K S Ho, MBBS(HK), FHKAM(Medicine), FHKAM(Family Medicine) Consultant, Elderly Health Services, Department of Health. Correspondence to : Dr R S Y Lee, Elderly Health Services, Department of Health, Room 3502, 35/F, Hopewell Centre, Wanchai, Hong Kong.
References
|
|