|
August 2003, Volume 25, No. 8
|
Update Article
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Management of miscarriage in general practiceC M Yan 忻財敏 HK Pract 2003;25:367-372 Summary Miscarriage is a common complication in early pregnancy. It is mostly idiopathic and the prognosis is usually good. The initial management may be provided by family physicians who, therefore, should have up-to-date knowledge of its management. Apart from the clinical management by history taking, physical examination and investigation, counselling and psychological support are also important in the care of patients suffering from miscarriage. The idea of pre-conception care is useful for women who are preparing for subsequent pregnancies after a miscarriage. In addition, referral to "early pregnancy assessment unit" by specialist is advisable in the next pregnancy. 摘要 在懷孕的初期,流產十分常見。流產的原因大多不明,但一般而言,是不會影響未來的孕娠。 家庭醫生應對流產的處理有正確的認識,以能為流產病人提供初步的處理。 除了臨床的檢查和化驗,適當的輔導和心理支持也同樣重要。 流產後及在再度懷孕之前,婦女應有充足的孕前準備。還有, 再度懷孕後,更應盡早到「早期懷孕評估診所」作檢驗。 Introduction Miscarriage is common. The overall rate is thought to be 50%.1 Clinically recognised pregnancy loss is estimated to be 12-15%.2 Management of miscarriage is commonly encountered by obstetricians and is not a rare scenario in the daily practice of the family physicians. A study from the United Kingdom reported that most miscarriage first presenting to family physicians would eventually be managed in hospital3 or in an early pregnancy assessment unit (EPAU). A wide spectrum of patterns of management were noted. But how many are evidence-based? Another study showed that women suffering from miscarriage were dissatisfied with the medical care provided by their family physicians.4 Miscarriage is conventionally treated by surgical evacuation of the uterus, but medical evacuation is now possible. Moreover, there is still a place for the expectant management which allows the spontaneous expulsion of the products of gestation. The modern-day family physician should be aware of these. Definitions The definition varies in different places. In Hong Kong, miscarriage is the spontaneous termination of a pregnancy or early loss of foetal tissue from the uterus before 28 completed weeks of pregnancy. Most are early, well before 12 weeks. Nowadays, "miscarriage" replaces "abortion" since the latter may imply termination of unwanted pregnancy. Missed abortion is referred to as silent or delayed miscarriage while incomplete and complete abortion is called incomplete and complete miscarriage respectively. In Chinese, there is no problem in differentiating miscarriage (流產,小產) and termination of pregnancy (人工流產,墮胎). First trimester miscarriage happens before the twelve week of gestation while second trimester miscarriage are those between twelve and twenty-eight weeks. Second trimester miscarriage is much less common than the first trimester - sporadic second trimester miscarriages occur in less than 5% of all pregnancy losses. Recurrent miscarriage (RM), previously called habitual abortion, is defined as the occurrence of three or more consecutive miscarriages. Aetiology Though miscarriages are categorised into first and second trimester, overlaps in their aetiology exist. The first trimester sporadic miscarriage is mostly idiopathic. Abnormal foetal chromosomal makeup is detected in at least 50% of these miscarriages (compared with 20% in the second trimester).5 Investigation is not warranted unless the miscarriage is recurrent. Since the incidence of spontaneous clinical pregnancy loss is about 15%, the calculated chance of RM should be about 0.34%. However, RM affects 1% of women. The discrepancy implies there are underlying causes in some cases of RM. About half of RM are idiopathic. The other causes include parental chromosomal abnormalities, antiphospholipid syndrome (APS), hormonal causes associated with oligomenorrhoea and structural anomalies such as uterine malformation and cervical incompetence. "Luteal phase defect" is defined as a defective corpus luteum with insufficient progesterone production. This concept of luteal phase defect is contentious because there is still no consensus as to how it should be diagnosed and whether treatment will improve pregnancy outcome. However, serum progesterone levels are not predictive of pregnancy outcome and there is no evidence to support the use of exogenous progesterone supplementation in early pregnancy.6,7 Currently, the focus is on thrombophilias, such as activated protein C resistance which is detected in a small number of women with RM. More evidence is awaited to establish its role. The aetiology of second trimester miscarriage include idiopathic causes, anti-phospholipid syndrome (APS), structural uterine anomalies, cervical incompetence and bacterial vaginosis. Diagnosis The diagnosis is usually made by ultrasonogram. Silent miscarriage is diagnosed if the gestational sac has a mean diameter greater than 20mm without evidence of an embryo or yolk sac, or if the embryo has a crown rump length greater than 6mm without evidence of foetal heart pulsations.8 Transvaginal ultrasonogram should always be employed if any doubt exists on transabdominal scanning. The distinction between incomplete and complete miscarriage relies on a combination of ultrasonographic and clinical features. It is difficult to make a diagnosis based on the morphology and thickness of the endometrial lining. Thick and heteroechogenic endometrial lining in a patient who is having heavy vaginal bleeding usually implies incomplete miscarriage while thin and uniform endometrial lining in whom who has little vaginal bleeding suggests complete miscarriage. Management of miscarriage Management starts with history and physical examination (Table 1). Ectopic pregnancy should always be considered as a differential diagnosis of miscarriage. History should include the date of last menstrual period, the usual menstrual cycle, method of contraception, date of pregnancy test(s) done, the details about vaginal bleeding and abdominal pain. The presence of shoulder tip pain may point to diaphragmatic irritation from intra-peritoneal bleeding in ectopic pregnancy. Physical examination may reveal pallor when there is severe vaginal or intra-abdominal bleeding. Pulse and blood pressure must be taken. The abdominal examination in miscarriage is usually unremarkable except when there is ruptured ectopic pregnancy which may give rise to guarding and rebound tenderness. On pelvic examination, a dilated cervical os suggests incomplete or inevitable miscarriage. Foetal tissue mass may be seen. Cervical excitation tenderness may be demonstrated with ectopic pregnancy. A bimanual examination should be done to assess the size of the uterus. Tenderness and mass in the adnexal region may be a feature of ectopic pregnancy.
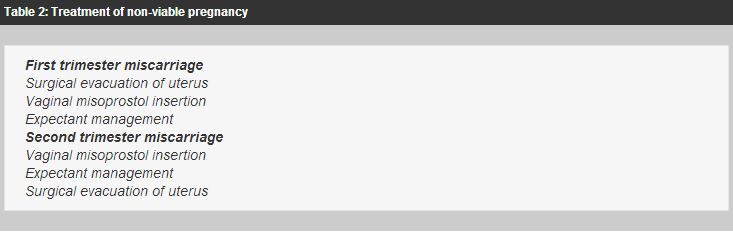
Pelvic ultrasonogram is essential. A threatened miscarriage is diagnosed when the cervical os is closed and the ultrasonogram demonstrates a viable pregnancy. Retained tissues will be demonstrated inside the uterus in incomplete miscarriage. Inevitable miscarriage is diagnosed when the internal cervical os is dilated, usually preceded by vaginal bleeding and lower abdominal pain. If the uterus is empty, the differential diagnoses will include complete miscarriage, ectopic pregnancy or very early intrauterine pregnancy. A further scan should be performed one week later. The urine pregnancy test is positive in miscarriage and ectopic pregnancy. Sometimes, serum human chorionic gonadotrophin level may need to be checked. Ectopic pregnancy must be ruled out if the serum human chorionic gonadotrophin level is higher than 2000iu/l, and the intrauterine gestational sac is not visible in the transvaginal pelvic ultrasonogram.9 A complete blood count is taken to detect anaemia in a patient who is bleeding vaginally. Rhesus status should also be ascertained if not yet known. Anti-D should be given to those non-immunised Rh negative women except where the foetus is viable and less than 12 weeks gestation.10 Options of treatment of non-viable pregnancy Threatened miscarriage is diagnosed if foetal viability is demonstrated. Septic miscarriage and heavy vaginal bleeding, will require urgent surgical evacuation of the uterus, otherwise three options are now available. They are expectant, medical and surgical management for non-viable pregnancy (silent and incomplete miscarriage). Expectant management for incomplete miscarriage is effective in about 80% where the endometrial lining is 15-50mm thick.11 It is less effective for silent miscarriage where about half of the patients may eventually require or request more active treatment.12 However, the patients have to wait for up to 4 weeks before the miscarriage is complete. Therefore, most of them still wish to have surgical evacuation of the uterus, which is 94% effective, but has a 8% risk of developing complications such as infection, uterine perforation and cervical laceration.13 Medical management is recently explored as an alternative. There were studies on the effectiveness of prostaglandins with or without mifepristone. It is difficult to conclude which regimen is better because there are non-uniformities in the selection criteria, choice and dosage of medication, and the definition of success. The success rate quoted was 61-92%.14-16 A commonly adopted regimen is 400mcg vaginal misoprostol, a prostaglandin E1 analogue. Caution should be exercised if the women have allergy to prostaglandins, cerebrovascular disease, coronary artery disease, hypotension or hypertension. Second trimester miscarriages are, in general, managed by medical method using similar misoprostol regimen since surgical treatment is more complicated in the second trimester. Expectant management is also an alternative (Table 2). However, one should be aware of the risk of coagulopathy with prolonged retention of non-viable foetal tissues for more than 4 weeks in late second trimester.
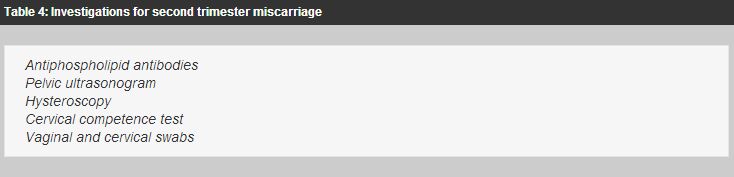
After a sporadic first trimester miscarriage, further investigations are generally not indicated. Investigations are suggested for RM as follows: parental karyotypes, antiphospholipid antibodies and pelvic ultrasonogram (Table 3). For second trimester miscarriage, the following tests may be performed: antiphospholipid antibodies, pelvic ultrasonogram, hysteroscopy and cervical competence test, and vaginal and cervical swabs (Table 4).
Counselling and support Counselling and psychological support is important to patients with miscarriage. Research has shown that psychological distress is reduced by appropriate counselling and support.17 The grief in miscarriage is comparable to that after stillbirth or the death of a relative. Miscarriage is increasingly being viewed as "perinatal bereavement".18 Moreover, the grief is a hidden one - others may never know the sufferer has been pregnant. Bereavement is particularly difficult because there is no visible child to mourn,19 no memories or shared life experiences20 and there is a lack of recognition of the significance of such loss by society.21,22 The suppression of appropriate mourning due to society's inhibition may cause further stress and life-long emotional consequences. Fears may also originate from concern about future fertility and surgery. The experience of miscarriage may also be a physically traumatic event involving pain, blood loss, hospitalisation and an operation. Hence, proper counselling and support from professionals are important. The knowledge of pregnant women about miscarriage was poor and there were a lot of misconceptions.23 Those misconceptions will add to the emotional disturbance. An information pamphlet on this topic for distribution to every patient with miscarriage is deemed to be useful. Prognosis and prevention The prognosis is related to the cause. In most cases where no cause is found, the prognosis is usually favourable, though it decreases with increasing maternal age and number of previous miscarriages.24 In RM, the prognosis is not affected by whether the RM is primary (no previous successful pregnancy) or secondary (previous successful pregnancies).25 Management is according to the cause. However these treatments are not evidence-based. At the moment, women with RM and APS are recommended to use low-dose aspirin 75mg daily throughout pregnancy. So far, the number of women in the treatment trials is small and there is continuing controversy about the value of heparin in addition to low-dose aspirin. Unless there is a history of maternal thrombosis, antenatal heparin is not routinely recommended.26 A randomised prospective study suggested that human chorionic gonadotrophin (HCG) therapy improved pregnancy outcome only in women with oligomenorrhoea and RM.27 Further extension of the study confirmed that those who did not receive HCG have a consistently poorer chance of success (59%) than women treated with HCG, who have a 75% chance of success.28 It is difficult to diagnose cervical incompetence objectively. The diagnosis is usually based on a history of recurrent second trimester miscarriages and an abnormal cervical competence test such as the retrograde cervical dilatation. A meta-analysis suggests a trend toward cervical cerclage reducing foetal losses before 34 weeks of gestation. It can be interpreted that 20 cervical cerclages are needed to prevent one case of miscarriage or preterm birth less than 34 weeks of gestation.29 For the majority with idiopathic cause, tender loving care is proven to be effective in the management of RM with a success rate of 86%.30 Pre-conception care Women are eager to know how to prepare for subsequent pregnancies. Though there are no specific strategies, something can be done before the next pregnancy is attempted. When a woman is seen for miscarriage, it is a good time to introduce the concept of pre-conception care.31 The past health, drug history, family history and social history are reviewed and screening tests are carried out to detect her reproductive risks. Susceptibility to Rubella infection may be discovered even with a history of prior vaccination. Rubella antibody levels may drop with time and so it is probably advisable to check antibody status before each pregnancy. Pregnancy should be avoided for one month after vaccination. At present, there is no evidence to support the use of vitamins or trace elements when planning a pregnancy except for folic acid, which can reduce the incidence of neural defect-affected pregnancies. It is recommended that women should take folic acid 400mcg daily from the time they decide to become pregnant till the twelfth week of gestation.32 There is much evidence that cigarette smoking has harmful effects on foetus and smoking remains one of the few potentially preventable factors associated with low birthweight and perinatal death. In those who cannot stop smoking, reduction should be the goal for all prospective mothers (Table 5).
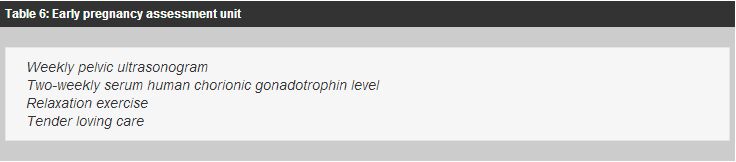
Management of subsequent pregnancy Family physicians should refer the women to a specialist or an EPAU early so that weekly ultrasonogram is done to provide assurance. The concept of gestational milestones as suggested by Farquharson is useful: the most perilous gestation for pregnant women with idiopathic RM is between 6 and 8 weeks and beyond 10 weeks the miscarriage rate is only 0.6%.33 Moreover, once the foetal heart activity is detectable, the anticipated pregnancy loss is 3%.34 In some centres, 2-weekly serum human chorionic gonadotrophin level is performed. A doubling time of 2 days or less is consistent with normal pregnancy. Relaxation exercise is also useful for the inevitably nervous sufferers of RM in the subsequent pregnancies.35 Of course, tender loving care and support from the staff in the EPAU is important (Table 6).
Conclusion Miscarriage is a common condition that family physicians should be prepared to manage. Management should be evidence-based and empirical treatments should be avoided because they may be unnecessary and even potentially harmful. Education and counselling are important in the holistic care for women with miscarriage. After the initial management provided by family physicians, referral for further management by gynaecologists is sometimes needed. Women should be introduced to the concept of pre-conception care. Key messages
C M Yan, MRCOG, FHKAM(O&G)
Senior Medical Officer, Department of Obstetrics and Gynaecology, United Christian Hospital. Correspondence to : Dr C M Yan, Department of Obstetrics and Gynaecology, United Christian Hospital, Kwun Tong, Kowloon, Hong Kong.
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||