|
October 2002, Volume 24, No. 10
|
uipate_2
|
|||||||||
An update on management of common paediatric respiratory emergenciesE Y T Chan 陳日東,D K K Ng 吳國強,P Y Chow 周博裕,C K L Kwok 郭嘉莉 HK Pract 2002;24:491-497 Summary Croup, acute bronchiolitis and asthma are the common causes of acute respiratory distress in children. Croup is a viral infection of the upper airway whereas acute bronchiolitis is that of the lower airway. Asthma is a partially or completely reversible obstruction of the bronchial tree secondary to inflammation. The prevalence of asthma in Hong Kong is rising, like other parts of the world. Croup and acute bronchiolitis account for 0.8% and 3.9% respectively of all admissions of children to hospitals under Hong Kong Hospital authority. All three diseases share one common clinical feature during acute presentation, i.e. respiratory distress. In this review, the causes, clinical features and current management of croup, acute bronchiolitis and asthma are discussed 摘要 哮吼、急性細支氣管炎和哮喘是兒童急性呼吸窘 迫的最常見病因。哮吼是病毒引起的上呼吸道感染;而急性細支氣管炎是病毒引起的下呼吸道感染。哮喘 則是繼發於炎症的支氣管樹的部份或完全的可逆性阻塞。同世界其他地區一樣,香港的哮喘患病率也在上 升。香港醫院管理局所屬的醫院內,哮吼和急性細支氣管炎分別佔兒童入院人數的 0.8%和3.9%。於急性發作期,三種疾病都有一個共同的臨床特徵,即呼吸 窘迫。本綜述討論了哮吼、急性細支氣管炎和哮喘的病因,臨床病史和目前的治療方法。 Introduction Respiratory distress is an alarming symptom in all patients. Life threatening events occur if the particular cause is not identified and managed appropriately. The commonest cause of respiratory distress in infants and toddlers are acute bronchiolitis and croup. For the older children and teenagers, asthma is the commonest cause of respiratory distress. Respiratory distress would be the commonest emergency condition in children that would occur in regular interval in general practice with a sizeable paediatric population. Optimal investigations and timely interventions are the keys to successful management. In this review, the current recommended management of croup, acute bronchiolitis and asthma are discussed. Foreign body aspiration would also be discussed briefly as it can mimic all three conditions. Croup Croup is a viral syndrome involving infection of the upper airway, characterised by the acute occurrence of inspiratory stridor and a barking cough. Symptoms tend to worsen at night. Common causative agents are parainfluenza virus types 1, 2 and 3. It mainly occurs in children, with 91% of cases occurring in children less than 5 years of age and most cases occurring before 2 years of age.1 The main pathology lies in the inflammation of the supraglottic, glottic and subglottic structures. The incidence of viral croup peaks in winter months. In Hong Kong, the male to female ratio was 2:1. Croup accounts for 0.70% and 0.81% of all hospitalisation in Hong Kong public hospitals in 1998 and 1999 respectively.2 Croup is diagnosed clinically ONLY after acute epiglottitis, foreign body aspiration, and bacterial tracheitis have been excluded.2 Epiglottitis is rare in Hong Kong. Clinical features include sudden onset of high fever, drooling of saliva, dysphagia, anxiety, and aphonia. The toxic appearance of epiglottitis should readily distinguish epiglottitis from croup. Haemophilus influenzae type B is the commonest cause of epiglottitis. Minimal disturbance of children should be observed and the patient should be referred for tracheal intubation under controlled setting in the operation theatre by an experienced anaesthetist. An experienced surgeon should be on stand-by for emergency tracheostomy. Bacterial tracheitis is an infection of the trachea leading to an ulcerated tracheal mucosa with thick purulent exudate. It is often a complication of croup. Clinical features include high fever, toxicity, inspiratory stridor, barking cough and respiratory distress. Staphylococcus aureus is the commonest bacterial pathogen. It is diagnosed by the typical appearance of the trachea visualised by flexible bronchoscopy. History of choking or gagging followed by an acute onset of stridor suggests the possibility of foreign body aspiration. Complete blood count and arterial blood gases are not necessary nor helpful in most cases of croup. Painful or unnecessary manipulation of young children may indeed aggravate the severity of croup.2,3 Hence, blood tests should be done only in severe cases.3 Neck x-ray is normal in 50% of croup patients. Typical radiographic findings include a narrowed air column in the subglottic area seen on the posteroanterior view, steeple sign, and over-distended hypopharynx on the lateral view. Radiographic findings, however, do not correlate well with clinical measures of severity of croup, and radiographic studies should be limited to children whose diagnoses are not clear and whose respiratory status is stable. A period of close observation helps to ascertain the diagnosis. Respiratory rate, heart rate and conscious state are useful clinical parameters. Monitoring of oxygen saturation is useful in moderate to severe case as hypoxaemia is an indication of respiratory compromise.4 Transcutaneous carbon dioxide pressure monitoring provides a useful parameter in severe cases.4,5 Scoring system for clinical severity is not necessary in routine clinical practice. Management Management includes regular monitoring for signs of deterioration, e.g. depressed conscious level, increased insucking of chest wall. Mild cases can be managed in the emergency department. Medications used in management of croup are summarised in Table 1. Parenteral or oral dexamethasone, 0.6mg/kg, is recommended for treatment of moderate to severe viral croup.6,7 One randomised controlled trial involving 120 children showed that lower doses of oral dexamethasone, 0.15mg/kg, 0.2mg/kg or 0.3mg/kg, was as effective as the conventional dose. However, patients on lower doses of dexamethasone were more likely to receive nebulised adrenaline.8 Hence, a single dose of 0.6mg/kg dexamethasone is recommended at present.
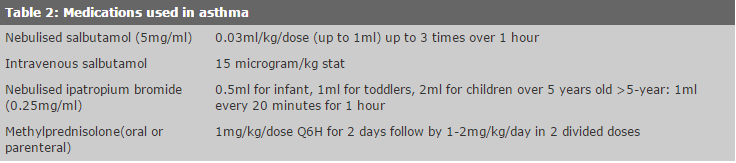
Nebulised budesonide (a single dose of 2mg) is a reasonable alternative.9-12 If the patient has vomiting, parental dexamethasone or nebulised budesonide is preferred. Nebulised adrenaline is useful as an initial treatment for immediate relief because of its vasoconstriction effect. Both racemic and L-isomer adrenaline are equally effective in temporarily decreasing the severity of croup. L-isomer adrenaline is preferred because of its lower cost and ready availability. A dose of 0.5ml/kg of 1:1000 L-adrenaline added to 3ml normal saline, a maximum dose of 2.5ml for children less than 4 years of age or 5 ml for children above 4 years old, is recommended.3 However, the effect is temporary and there is a possibility of relapse. Patients should not be discharged based on their initial improvement after nebulised adrenaline. Concomitant dexamethasone or nebulised budesonide must be given. Moreover, nebulised adrenaline should be used with caution in children with pre-existing cardiac disease for fear of causing myocardial infarction.13 Routine oxygen supplement is not necessary but it should be given if the child has desaturation or progressive tachypnoea, tachycardia, cyanosis and laboured breathing. Parenteral fluid or naso-gastric tube feeding is recommended for children with respiratory distress to reduce the likelihood of aspiration during oral feeding. Antibiotic is not recommended unless bacterial infection is clinically likely to be present. Intubation is rarely required but the patient should be timely intubated if necessary. Size of the endotracheal tube with a diameter of 0.5 to 1mm less than predicted is recommended. The use of humidified air and the routine use of chest physiotherapy are not recommended. In cases of mild croup, reassurance should be given. Dexamethasone should be given to patients with stridor at rest and patient should be reviewed within 2-4 hours after the therapy. In patients with respiratory distress on presentation or failure to improve after treatment, nebulised adrenaline should be given and hospital referral is mandatory. Bronchiolitis Bronchiolitis is a viral induced acute bronchiolar inflammation with signs of lower airway obstruction. The commonest pathogen is respiratory syncytial virus (RSV). Other pathogens include parainfluenza, influenza and adenovirus. Dual infection with other organisms such as Chlamydia trachomatis or Mycoplasma pneumoniae occurs in about 5-10% of RSV lower respiratory tract infection.14 It is one of the major causes of hospital admissions in infants under the age of one year. >From 1997 through 1999, nearly 10,000 children were discharged from public hospitals with the diagnosis of acute bronchiolitis. This represented 5% of total paediatric discharge from all hospitals under the Hong Kong Hospital Authority.15 The peak incidence was found to occur during the summer months in Hong Kong.15,16 Bronchiolitis usually presents with an initial picture of upper respiratory tract infection. The child may appear restless and tachypnoeic. Cyanosis may be noticed. Examination of the chest may reveal diffuse inspiratory crackles and/or expiratory wheezes. Investigations often add little to management. Immunofluorescent antibody test or enzyme linked immunosorbent assays provide rapid identification of the virus in nasopharyngeal aspirate. Chest x-ray is helpful if the diagnosis is in doubt or if there is a suspicion of secondary bacterial infection. Electrolyte levels should be performed in severe cases, as syndrome of inappropriate release of antidiuretic hormone may occur. Pulse oximetry is simple and safe for monitoring the oxygen saturation.17 Management Bronchiolitis is a self-limiting illness. Careful monitoring of the infant for hypoxia, apnoea and exhaustion is important. The mainstay of treatment is supportive. Properly heated and humidified oxygen should be given to maintain a minimum oxygen saturation of 95%.18 A balance between risk of dehydration and the possibility of fluid overload and inappropriate secretion of antidiuretic hormone should be attained.19 The role of bronchodilators is controversial. Nebulised or subcutaneous adrenaline was shown to improve oxygen saturation and clinical scores.20,21 Menon et al showed that nebulised adrenaline (3ml of 1:1000 adrenaline given by nebuliser with continuous flow of 5-6L/min oxygen) is superior to nebulised ventolin (0.3ml of 5mg/ml ventolin).22 Kellner et al performed a meta-analysis of studies involving salbutamol, epinephrine and ipratropium bromide in children with acute bronchiolitis and concluded that these bronchodilators only produced modest short term improvement in clinical scores and this small benefit should be weighed against the costs of these agents.23 In the authors' department, nebulised ipratropium bromide was arbitrarily chosen as the first agent to use in children with wheeze due to acute bronchiolitis. It would be continued if wheeze decreased after use. If there was no response, the second agent to be tried was nebulised salbutamol. The third agent to be tried was nebulised epinephrine. If either salbutamol or ipratropium was found to be effective, it would be given by metered-dose inhaler (MDI) with a spacer device the day after admission. The switch was based on the fact that MDI with a spacer was as good as a nebuliser.24,25 If all were not found to be effective, the parents would be informed and be assured that supportive care with fluid, nutrition and oxygen would ensure recovery in almost all children. An audit of this practice was conducted in the authors' department. 50 children with bronchiolitis were reviewed. 47 were found to be responsive to ipratropium bromide and three failed to respond. Of these three children, two responded to salbutamol. The last child responded to nebulised epinephrine (unpublished data). This preliminary data was encouraging and further randomised controlled trials are warranted in Hong Kong. As a rule, cough mixture was not given in the authors' department for lack of efficacy and dubious safety. The use of steroid in bronchiolitis showed conflicting evidence though the use is widespread in North America.17 A double-blind randomised, placebo-controlled trial involving 70 children concluded that outpatients with moderate-to-severe acute bronchiolitis derived significant clinical and hospitalisation benefit from oral dexamethasone, 1mg/kg, treatment in the initial 4 hours of therapy.26 Routine use of antibiotic did not improve the clinical outcome and secondary bacterial infection was unusual.27 Asthma Asthma is characterised by recurrent episodes of dyspnoea and/or cough and/or wheeze. In Hong Kong, it is the commonest chronic disease affecting children. The prevalence was 6.0% in children between 3 and 10 years of age in Hong Kong28 and 11% in 13 and 14 years old age group.29 Diagnosis of asthma is mainly based on history and symptoms. There is no single diagnostic test for asthma. Spirometry and bronchial challenge test are useful tools in the overall management of suspected and confirmed cases of asthma.30 The severity of asthma can be classified as mild, moderate, severe and life-threatening. An attack is mild if the child has wheeze without respiratory distress, his peak expiratory flow rate (PEFR) is more than 80% of the predicted value or personal best, or pulse oximetry shows oxygen saturation >95% in room air. An attack is moderate if the child has wheeze with evidence of respiratory distress, use of accessory muscles, tachypnoea ,tachycardia, agitation and impaired speech in joined-up phrases or PEFR between 50-80% of the predicted value or personal best or pulse oximetry shows oxygen saturation between 91-95% in room air. An attack is severe if the child is not able to speak through phrases, not able to feed, has worsening of features listed in moderate attack or PEFR is <50% predicted or personal best or pulse oximetry is less than 91%.31 A post-bronchodilator oxygen saturation of less than 91% was found to be the best predictor for a severe attack.32 Management of acute asthma In clinical practice, the basic principles of treatment include early recognition and treatment by the patients themselves or their caretaker, preferably aided by an individually written action plan, with emphasis on symptoms and alterations in peak expiratory flow rate.30 Heated humidified oxygen should be used to keep oxygen saturation of more than 92%. Medications used in acute asthmatic attack are summarised in Table 2.
Salbutamol (5mg/ml) at a dose of 0.03ml/kg/dose (minimum 0.25ml, maximum 1ml) which should be added to normal saline to make up a final volume of 3ml, and driven for 3 doses by oxygen flowing at 6-8 L/min every 20 minutes is the most promising regime.33 For mild to moderate asthma, salbutamol can also be given by an MDI, with up to ten puffs through a spacer, with or without a mask, at the rate of one puff every 15-30 seconds. In severe asthma, intravenous infusion of salbutamol 15mcg/kg given over 10 minutes on admission was shown to result in a shorter duration of oxygen dependency and recovery time, without any difference in side effect.34 Ipatropium bromide was shown to have synergistic bronchodilator effect.35 The recommended dose is 0.5ml (0.25mg/ml) for infants, 1ml for toddlers and 2ml for children over 5 years of age. In severe case, for children older than 5years of age, it is safe to be given at a dose 0.25mg every 20mins for 1 hour.36 Corticosteroid is recommended in moderate asthmatic attack with incomplete therapeutic response or a relapse of symptoms within four hours after bronchodilator therapy and in severe asthmatic attack. Early use is important as it takes around six hours to demonstrate effect. Methylprednisolone is preferred as it has less mineralcorticoid effect compared with hydrocortisone. The dosage is 1mg/kg every six hours for two days followed by 1-2mg/kg/day, in two divided doses for 3 days. Tapering of corticosteroid dosage is not necessary. Use of montelukast, a leukotriene receptor antagonist, improves the forced expiratory flow volume in one second in patients with chronic asthma who are six years of age or older. A pilot study showed that IV montelukast has a rapid onset of action, (15 minutes), and prolonged duration of action, (24 hours). It might have a role in the management of acute asthma.37 Use of aminophylline infusion (5mg/kg over 20 minutes followed by 1mg/kg/hr iv) in severe asthma showed conflicting evidence and their use was not recommended in the Second Expert Panel of the Management of asthma (NIH) in 1997.31 Use of magnesium in acute asthma in adult showed an increase in FEV1, but several studies showed varied results and magnesium does not yet have a role in the initial regimen of therapies used in asthma.38 Chest physiotherapy and mucolytic agents are not recommended as the latter may actually worsen airflow obstruction. Education about asthma after recovery is the most important step to ensure better control of asthma.39 In mild to moderate asthmatic attacks, patients can be managed as outpatients with bronchodilators with or without steroids. Reassessment after initial therapy is important. Pre- and post-treatment PEFR, pulse oximetry and the frequency of bronchodilator use can help determine whether the patient requires hospital admission in the clinic. An emergency department prospective cohort study of 278 children found five variables to be associated with a long course of therapy: previous intensive care unit admission, baseline oxygen saturation 92%, asthma score 6/9, oxygen saturation 92% at 4 hours and use of hourly salbutamol nebulisation in the initial four hours. A combination of three or more factors predicted a long duration of frequent bronchodilator requirement and suggested hospitalisation.40 Foreign body aspiration Foreign body aspiration can present with life-threatening upper airway obstruction or recurrent wheeze.41 The peak incidence of foreign body aspiration occurs during the second year of life in the child group. In one review,42 the commonest presenting symptom is the penetration syndrome, defined as a sudden onset of choking and intractable cough with or without vomiting, seen in 49% of patients; the second most common symptom is cough (37%); breathlessness and wheezing are seen in 26% of patients. Hence, careful history taking for choking is very important in any child with respiratory distress. In children, most foreign bodies are found in the proximal airways, i.e. larynx, trachea, and main stem bronchi. Chest x-ray may not be helpful as most aspirated foreign bodies are radioluscent. Referral to the paediatric department is mandatory if the diagnosis is suspected as all cases would require endoscopic examination of the airway.42 Conclusion Respiratory distress is one of the few emergencies faced by family medicine physicians. It is important for family physicians to acquire a working knowledge in managing respiratory distress secondary to asthma, acute bronchiolitis and croup. Sophisticated investigations are usually not necessary. With appropriate treatment in the family clinic, a lot of children will not need to be admitted to hospitals. Review after initial therapy would be helpful in most of the cases. If the diagnosis is in doubt or respiratory distress persists, they should be referred to paediatricians for further management. Life-threatening conditions should be recognised and appropriate first line treatment given before timely referral to the emergency department.
E Y T Chan, MBBS(HK)
D K K Ng, M Med Sc, FRCP, FHKAM(Paed)
P Y Chow, MBChB, MRCP, DCH Senior Medical Officer, Department of Paediatrics, Kwong Wah Hospital. Correspondence to: Dr D K K Ng, , Department of Paediatrics, Kwong Wah Hospital, Kowloon, Hong Kong. References
|
||||||||||