|
September 2001, Volume 23, No. 9
|
Update Articles
|
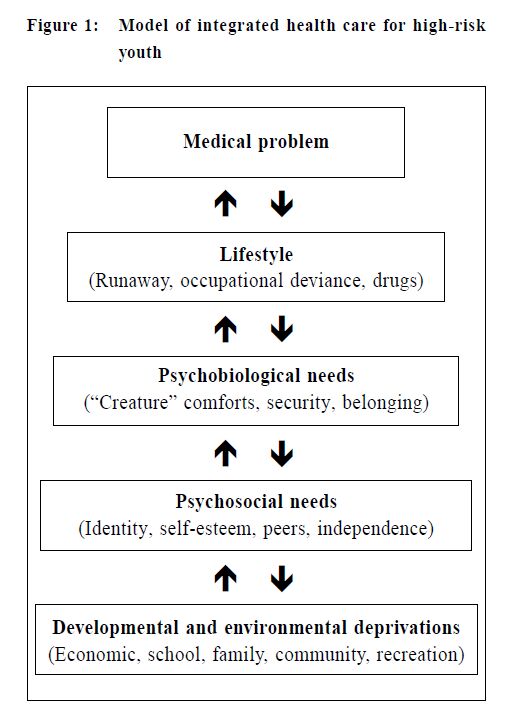
Adolescent medicine and the effective clinical consultation of adolescentsP C H Cheung 張志雄 HK Pract 2001;23:382-389 Summary Successful provision of health care to adolescents entails a sound knowledge of their growth and development. One needs to be able to understand their health concerns in the context of their environment. The clinical encounter between a clinician and an adolescent draws on specific skills on the part of the clinician and the adoption of a developmentally appropriate consultation model. The professional attitude of the clinician is a significant determining factor for the successful consultation. 摘要 要成功地為青少年提供醫療服務,必須對他們的 生長和發育有充份的認識。醫生應從他們的角度理解 問題,有專門的技巧,並採用適合青少年發育特點的 診症方式。醫生的專業態度也是決定診症成功與否的 重要因素。 Adolescent medicine and adolescent health problems "Adolescent Medicine" applies to the health care, professional training, health research, and advocacy related to persons age 10 to 25 years. It applies to the provision of both primary and specialty care.1 Adolescent health problems are diverse. The multi-faceted nature of their problems often necessitates the collaboration of multiple professionals such as the medical, educational, social work, law enforcement agencies, etc. Adolescent medicine is one of the paediatric subspecialties and its syllabus has been laid out by the Hong Kong College of Paediatricians.2 Local statistics on adolescent health parameters can be obtained from various organisations but these tend to concentrate on their own areas of interest.3-6 With reference to the local situation, valuable expertise such as the approach to adolescent health care has been instigated,7 and a hospital-based adolescent health profile has been documented in the past.8 Some of the basic principles of adolescent growth and development will be covered in the first half of this paper, followed by the more practical aspects of clinical consultation with adolescents. Adolescent health issues in relation to Growth and Development The following is an attempt to describe, from clinical observations, some of the adolescent health issues in the context of their growth and development, i.e. physical growth, cognition, self-identity, family, peers and sexuality. Children's Growth and Development concentrates on the maturational process of a child with respect to its inherent potential and its interaction with the environment. Growth is an increase in the size of a body structure. Development is an increase in the complexity of structure and function. Childhood development includes the following majors areas: gross motor, fine motor and vision, hearing and speech, social and intellectual development. Adolescent development takes on a similar perspective. Besides physical growth, an understanding of the psychosocial development is needed. Understanding of adolescent health problems requires a model based on the adolescent's growth and development. One such health care model suggests that any developmental and environmental deprivations leads to the unmet bio-psycho-social needs of the adolescent. This results in lifestyle changes that are manifest as medical problems.9 The end result is the medical manifestation of problems like substance abuse, mental health problems, medical complaints, sexuality-related medical concerns, victimisation and abuse, which then serve as the entry points into the care system. (Figure 1)
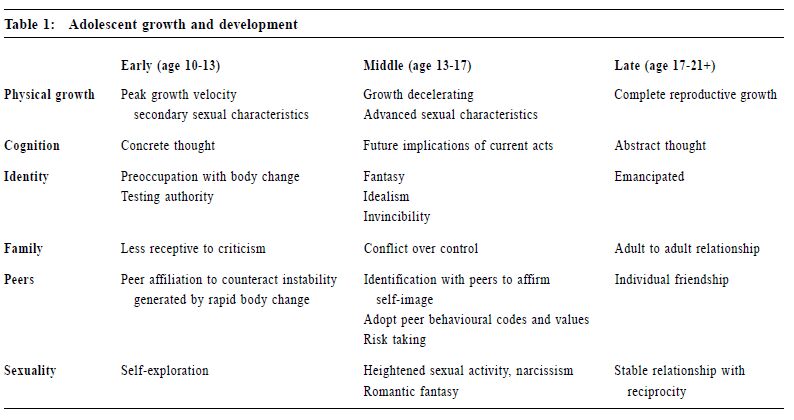
In the clinical encounter, outcome is invariably affected adversely if a practitioner only focuses on a single presenting symptom. Health problems should be interpreted and managed in the context of the adolescent's surroundings. These include his family, school (work) and peers. A knowledge of adolescent development allows one to grasp, comprehend and interpret the adolescent's thinking process, behavioural manners and their ensuing consequences; very much like putting together a jigsaw puzzle. Further, indicators of successful intervention and innovative strategies in the preventive health and specialist care of adolescents are based on such knowledge.10 Task of adolescence The three main tasks11 of adolescence are emancipation, identity formation and assumption of functional roles. An adolescent negotiates through several areas to achieve these tasks. These include physical growth, cognition, identity, family, peers and sexuality. There are special characteristics in each of these spheres in the three stages of early, middle and late adolescence. These are summarised in Table 1.
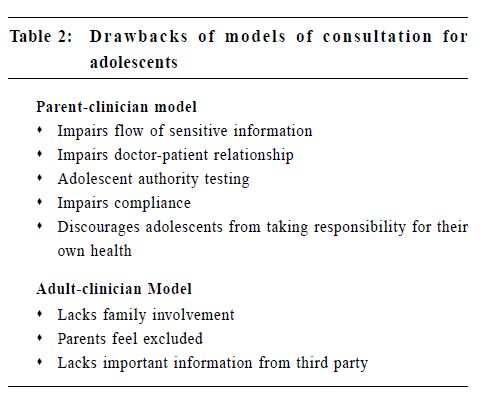
Physical growth Changes in hormonal profile in adolescence lead to rapid physical growth. Adolescents are sensitised to their bodily changes such as growth in stature, penis, breast and body hair, nocturnal emission, menstruation, advent of sexual feelings and behaviours like masturbation. This preoccupation and self-exploration often leads to the comparison of self with peers. Apprehension arises. The ensuing uncertainty, and may be unfound guilt are often handled by the adolescent alone. The capacity and degree of comfort of the average family in handling such pubertal issues seems to be limited. They may present to the health professionals with symptoms in disguise. Examples include scrotal pain in an adolescent concerned with his masturbation, chest pain in a pubertal boy with gynaecomastia, or abdominal pain in a teenage girl who recently became sexually active. Misinformation from the media and peers on health concerns often cultivate a strong belief on the part of the adolescent. This incorrect belief is often firmly held, and when challenged with health education will be met with resistance. Another observation is the newly re-defined meaning of health. Market-driven media often portray health as equivalent to beauty. The implication is that in order to achieve beauty or to stay healthy, there has to be a persistent pursuit to attain body figures as portrayed by various models. This leads to the limitation of adequate caloric intake and improper proportioning of essential food components required for growth. The recent surge in the number of eating disorders rightly prompted us to review the very many synthesising biopsycho- social factors. Many are using "healthy products" labelled as natural foods in a "therapeutic" manner, taking laxatives improperly; having purging behaviours, relentlessly exercising themselves beyond their physical capacity, resulting in bodily harm. Cognition With their new cognitive ability, adolescents are able to think about thinking, either their own or other person's thinking. But with the rapid development of intellect and the tendency to become self-centered, mistake is often made that they assume others are thinking what they are thinking about. This is most pronounced in early adolescence and is termed "Imaginary Audience", a belief that they are on stage.12 This thinking process contributes to the construction of "Personal Fable", a belief that they must be special in some way if everyone is watching them. This sense of invulnerability is also most pronounced in early adolescence and evolves into middle adolescence as immortality and a sense of omnipotence. A study revealed that 40% of adolescents were confident of being able to try soft drugs without getting addicted.13 Before full maturity of cognition, there is difficulty and often denial in relating the long-term consequences to present actions. In this context, many risk-taking behaviours in adolescence can be explained. Injuries and accidents, drug use, smoking, premarital sexual intercourse, pregnancy and sexually transmitted diseases are key problems relating to these developmental characteristics. Self-identity and family Achieving abstract thinking abilities from concrete thinking is another milestone of adolescence.14 This mental ability enhances the construction of self-identity. With this cognitive expansion, the adolescent is able to construct ideals. This includes ideal parents, families and the wider society. The process of development of self value and moral systems often results in authority and limit testing. This brings challenges and creates tensions to the families and teachers. Furthermore, adolescents readily perceive peers as a source of comfort and affection superior to that from home. With early childhood maladjustment, poor family functionality, lack of parental trust and respect for adolescents, any additional environmental stressors may result in health problems like physical abuse, eating disorders, self-harm behaviour, runaways and the like. Peers Emancipation is at its peak in early and middle adolescence. Any attempt at moderation of this distancing threatens full independence. Peer conformity in dress, behavioural codes, values, etc, is a prerequisite for group acceptance. Experimentation and exploration of different experiences takes place in the permitting environment of the peer group. Again, risk taking is a phenomenon with the initiation of unhealthy lifestyles that may take their toll in adulthood. Nevertheless, peer pressure may exert positive influences in academic, sport, religious or cultural arenas. Sex In early adolescence, there is a strong emotional, tender feeling towards peers of the same sex, and also experimental sexual play. For most adolescents, this is part of the developmental process leading to heterosexual identity. For some, such tender feelings are equated with homosexual feelings, with manifestation of anxiety, confusion or panic. Towards later adolescence, sexual values and sexual feelings are more evidently defined. Homosexuality is a topic on its own. Nevertheless, the development of homosexuality takes its course from early childhood, through adolescence to adulthood. Many homosexual youths report a feeling of being different from their peers from early childhood,15 and age of homosexual self-identification has been dropping according to overseas studies.16,17 Clinical consultation of adolescents Clinical consultation of an adolescent takes on a different perspective to that of a child or a mature adult. Management of children in the office setting involves communication mainly between the clinician and the caretaker who shares the history, decision and management while the child takes on a passive role. This is a Parent-Clinician model. Understandably, an Adult- Clinician model is adopted for mature adults. Clinicians should try to avoid treating adolescents as large but dependent children or small but self-sufficient adults. The drawbacks of this are summarised in Table 2. While one would adopt the Parent-Clinician model for early adolescents with simple straightforward ailments and the Adult-Clinician model for the emancipated late adolescents, it is evident from the above discussion that a different approach to consultation is needed especially for the middle adolescents.
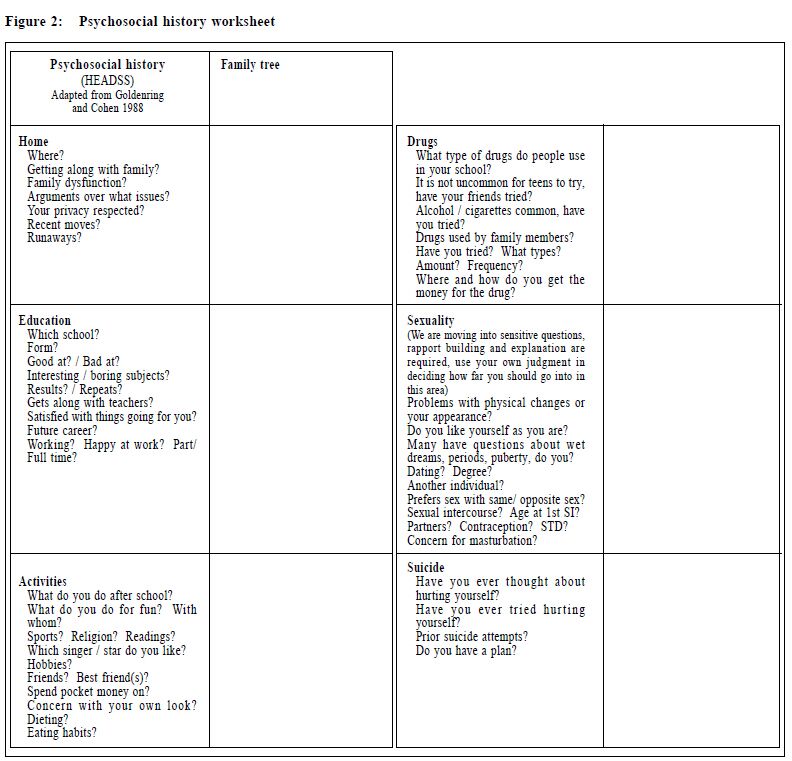
The Adolescent-focused consultation model There are recommendations on the access to health care for adolescents based on many surveys, one of which is promulgated by the Society of Adolescent Medicine.18 It concentrates on seven areas: availability, visibility, quality, confidentiality, affordability, flexibility and coordination. The wordings of these seven areas are selfexplanatory and the principle can be applied to the office settings of any primary care physician. Without discussing the clinic office management such as scheduling of appointments, fee structure, office decor, staff training and mannerism, we concentrate on the model of clinical consultation and an example of this model is described below. This Adolescent-Focused consultation model is particularly useful for those adolescents who test authority strongly to strive for independence, or for those with chronic illnesses who need to be assisted to achieve self-sufficiency, or for those enmeshed families whose parents experience difficulty in releasing the ties to their children. This can also be applied to those adolescents with confidential health issues and issues with psychosocial components. From his entrance into the doctor's room, the adolescent is treated as the primary user and all the clinician's communicative cues like greeting, seating, and other forms of body language are directed primarily to the adolescent, with the parent at a secondary level. After the health concern is elicited, the parents are asked to leave the room. Many parents respect their child's need for autonomy and confidentiality. The ensuing history, examination and formulation of the management plan are carried out in a manner that necessitates specific skills and this will be described in the latter part of this paper. Towards the end of the consultation, the parents are invited back into the room and the management plan is reviewed, preferably by the adolescent himself or herself so as to clarify any unclear points. This will boost the adolescent's confidence as well as facilitate adherence to the management plan. Skills in the clinical consultation of adolescents Rapport and trust-building are the essential elements contributing to the successful consultation. Adolescents are convinced that nobody understands them or takes their concerns seriously. On the other hand, they want to talk to somebody desperately, but the information will not be forth-coming until they feel you are trustworthy. This begins with good communication and requires good rapport. Rapport is a cooperative and harmonious interaction between people. It depends on how competent and trustworthy you are as a health professional. Establishing a private environment and avoiding interruptions during the consultation will go a long way in improving your quality of care to adolescents. One major pitfall to avoid in seeing adolescents is to adopt a judgmental attitude, especially in giving your advice on their health behaviours. Evaluation of patients should not be affected by one's personal feelings, attitudes, judgments, values or religious beliefs. Criticising their acts and not their person, providing a non-threatening environment to solve problems in a non-confrontational manner is the key to success. There is much information that can be gained by observation alone – their attire, facial expression, mannerisms and parent-adolescent interaction, not to mention the basic skill of being able to listen. As a general rule, the benefit you obtained in making the clinical diagnosis is proportional to the time spent by the adolescent in talking, rather than yours. Medical jargon is to be avoided as well as a trendy teenage attire on the part of the practitioner who wants to identify desperately with the adolescent. Prompting them to talk For teenagers who have difficulty in relating to you about their history, or for those who answer "I don't know" to your open-ended questions, there are a few things you can try. It is easier for them to relate certain symptom to specific events. "Did your chest discomfort start before or after last Christmas?" Another example is to ask them to rate their symptoms on a scale of ten, one being the best and ten being the worst. Another technique is to ask them to compare. The question, "How would you compare your home with that of your best friend?", may prompt an answer like, "I envy my friends because my father has beaten me badly for coming home late and I have ran away from home a couple of times because of this". Their thoughts can be helped to surface by asking the magic question, "If you have 3 wishes to change your health now, what would they be?" A teenager with an eating disorder may respond "I wish that I did not have to argue with my family about what I should be eating; that I can have a bowel motion every day; and that I can get rid of the calories I consumed". You may also give them permission to talk: "It is quite normal for boys of your age to masturbate, do you?" Teenagers like to be friends with those with the same psychosocial needs so information can be obtained by asking about what's happening to their friends. You can use a cascade of questions by projecting the undesirable teenage behaviours to their friends – "Do students from your school do drugs? Any of your friends do drugs? What about yourself?" There are many other techniques one can adopt in the clinical consultation. These include a skillful use of reflection to create empathy, use of summary and restatement to clarify your understanding of what the teen has just said. Another important point clinicians should bear in mind is that the interview should be carried out in a developmentally appropriate manner. A tool for the teenage interview An adolescent often seems to present with many health issues to be resolved in one consultation. The clinician may be lost as to what to tackle first, or the adolescent may have some vague symptoms, which often simply do not fit in well with the clinician's scientificformula. These difficult clinical situations can be tackled by adhering to a standardised interview format. As described before, one often needs to interpret adolescent's health in the context of their environment. This psychosocial history should form part of the adolescent medical history and is carried out after the details of the medical complaints are elicited. A simple and easy-tofollow format is by the acronym 'HEADSS'19 which stands for Home, Education, Activity, Drugs, Sexuality and Suicide. The sequence of topics is arranged in such a way that it moves from the simple and factual aspects of the adolescent's life into the more sensitive areas. It also allows rapport building in the initial stage of the interview. The adolescent is reassured that the questions are applied to all teenagers. The clinician can say something like this: "I am going to ask you some questions concerning your every-day life. This will help me in understanding and caring for you better. The questions I am asking you I will ask every adolescent. And some of the questions I ask you do not necessarily mean that I think you would act like that". An example worksheet is in Figure 2.
Confidentiality A concept of conditional confidentiality is required in which not all of the issues covered can be kept confidential by the clinician. The clinician may say, "You may choose not to answer any of the questions if you do not want to and I won't feel annoyed. But what you have told me, I will keep confidential. However, there are a few situations in which I cannot do this for you. These are: if you tell me that you have been hurt before in any way, or if you are thinking of hurting someone or if you want to hurt yourself. In these situations, for the sake of your own health I may need to share the information with other health workers". There are other aspects of confidentiality that simply cannot be covered in this article, suffice to say that it is an important aspect of adolescent health care that often taxes the clinician's patience. Structuring the clinical encounter The above paragraphs have covered some of the basic areas on knowledge, skills and attitudes required in the provision of health care to adolescents. For obvious reasons, one needs to formulate the clinical encounter to be efficient and one could consider the following structure:20
Conclusion Adolescent medicine applies to the provision of primary and specialty care. Adolescent health problems are diverse and multi-faceted. This requires a collaborative approach from multiple disciplines. Clinicians can do their part well in the consultation by gaining a sound knowledge of adolescent growth and development. Fostering a non-judgmental attitude to care and developing a structured adolescent-focused consultation model are essential elements for the clinical encounter. Interview skills can be mastered with perseverance. Key messages
P C H Cheung, DCH, Dip Obs, FRNZCGP, FHKAM(Paed)
Senior Medical Officer, Department of Paediatrics and Adolescent Medicine, United Christian Hospital. Correspondence to : Dr P C H Cheung, Department of Paediatrics and Adolescent Medicine, United Christian Hospital, Kwun Tong, Kowloon, Hong Kong.
References
|
|