|
May 2001, Volume 23, No. 5
|
Update Articles
|
Common occupational diseases in Hong KongM Y Ho 何孟儀, W K Lo 羅偉基 HK Pract 2001;23:208-211 Summary
Objectives: To review the confirmed cases of occupational diseases recorded
in Hong Kong from 1995 to 1999.
摘要
目的: 香港自1995 至1999 年已證實的職業病個案的探討。
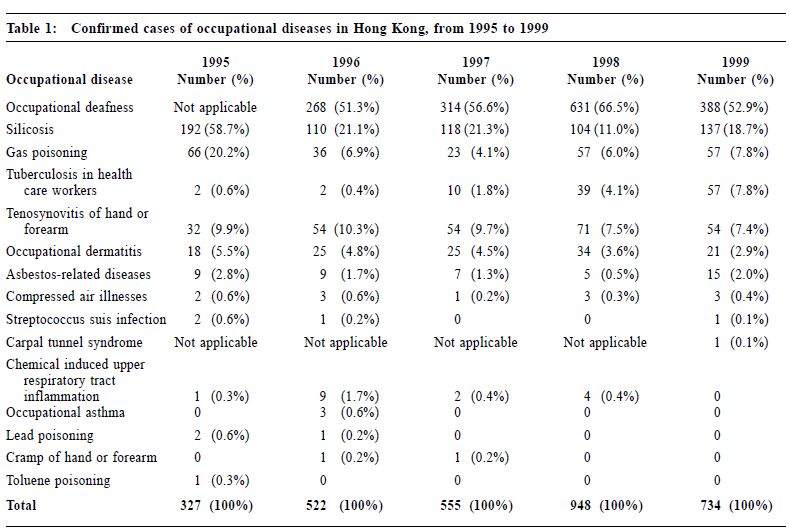
Introduction This paper aims to review the confirmed cases of occupational diseases in Hong Kong from 1995 to 1999 and to remind all medical practitioners to notify suspected cases to the Commissioner for Labour. There are a total of 49 notifiable occupational diseases under the Occupational Safety and Health Ordinance. All medical practitioners are required to notify the Commissioner for Labour of the occurrence of such cases. Notification of occupational diseases is important for controlling such diseases and monitoring the health status of our working population. To facilitate medical practitioners to fulfil the requirement, the "Guidance Notes on the Diagnosis of Notifiable Occupational Diseases" was published in 1997. It has been put up onto the web site: http://www.info.gov.hk/labour/public/oh/GuideD99.pdf Patients suffering from the notifiable occupational diseases are eligible for compensation under three d i fferent ordinances, namely the Employees' Compensation Ordinance, the Pneumoconiosis (Compensation) Ordinance and the Occupational Deafness (Compensation) Ordinance, provided that the compensation criteria are fulfilled. Confirmed cases of occupational diseases from 1995 to 1999 Table 1 shows the number of confirmed cases of occupational diseases from 1995 to 1999 in Hong Kong. The total number of confirmed cases increased from 327 in 1995 to 948 in 1998. The increase was mainly due to the addition of occupational deafness cases to the list of compensable occupational diseases, on the enactment of Occupational Deafness (Compensation) Ordinance on 1 July 1995. The most common occupational diseases reported in Hong Kong in the past five years were occupational deafness, silicosis, gas poisoning, tuberculosis in health care workers, tenosynovitis of hands and forearms, and occupational dermatitis. They accounted for more than 94% of all occupational diseases reported each year.
Occupational deafness is the irrever s i b le sensorineural hearing loss caused by prolonged exposure to excessive noise at work. The hearing impairment usually commences at 4-6 kHz but extends to other frequencies with continued exposure.1 The diagnostic criteria for occupational deafness were in line with the compensation criteria made under the Occupational Deafness (Compensation) Ordinance. To be eligible for compensation, workers have to fulfil certain disability and occupational requirements. Initially when the Occupational Deafness (Compensation) Ordinance was enacted in 1995, the disability and occupational requirements were more stringent. Workers should have sensorineural hearing loss amounting to at least 50 dB averaged over 1, 2 and 3 kHz frequencies in each ear with the hearing loss in at least one ear due to noise. Workers should have at least 10 years of employment in aggregate in any of the 17 specified noisy occupations before they were entitled for compensation. Occupational requirements are necessary as there are many causes of sensorineural hearing loss and occupational noise-induced hearing loss is only the most common one. With effect from 30 June 1997, the ordinance has been amended and the criteria for compensation have been relaxed to enable workers suffering from the minimum hearing impairment of 40 dB in both ears to receive compensation. Moreover, eight more specified noisy occupations have been added and the minimal employment period in four occupations with daily personal noise exposure of 100 dB have been shortened to five years. Occupational deafness accounted for more than half of the total number of occupational diseases each year from 1996. The actual number of confirmed cases in 1998 was 631 which was twice the number of 1997. The abrupt increase was believed to be related to the change in compensation criteria. In the financial year 1998-99, 44% of the successful claimants had milder hearing loss with level between 40 - 49 dB in their better ear.2 In 1999, the number of confirmed cases dropped to 388 because most of the cases accumulated in the past years had been identified and their compensation payments settled. Silicosis is a chronic progressive fibrotic lung disease caused by inhalation and deposition of dust containing free silica. All silicosis cases were confirmed by the Pneumoconiosis Medical Board comprising two chest physicians and one occupational health officer. More than 100 cases were confirmed each year. Over 90% of the patients who suffered from silicosis worked in construction sites or quarries.3 About half of them had been involved in caisson operations where the silica concentration in air had been very high. Other occupations related to silicosis in Hong Kong were jade polishing, enamel or ceramics making, tombstone work and iron refining.3 In 1995, the Building Ordinance was amended to prohibit the use of open hand-dug caissons unless no alternative method was feasible. Since then, the number of caissons used for foundation-pier construction has decreased significantly. It is expected that the trend of silicosis cases will be quite stable in the next few years and will decrease gradually. When the Occupational Health Service receives notifications of the occurrence of gassing incidents in workplaces, the occupational health officer and the occupational hygienists will jointly investigate the incidents at the scene and collect medical information of the victims immediately. The aims of investigations are to identify the causes and to undertake remedial actions in the workplaces. The number of victims who suffered from gas poisoning from 1995 to 1999 was shown in Table 1. The occurrence of gassing incidents was quite variable and the number of victims in each incident differed. Less than 10 gas poisoning incidents occurred each year. Most gassing incidents occurred in underground confined spaces. Hydrogen sulphide, carbon monoxide and oxygen deficiency were usually identified to be the causative agents. Causative agents identified in other gassing incidents in the past few years included ammonia gas, chlorine gas, nitrogen oxides, vapour of organic acids and organic solvents. Sometimes the causative gas could not be identified as the rescuing operations including the flushing with outside fresh air disturbed the air environment inside the confined spaces. The majority of victims only suffered from eye and upper respiratory tract irritation with full recovery. Five fatal gas poisonings were recorded in the period from 1995 to 1999. The incidence of tuberculosis is quite high in Hong Kong. It is to be expected that many health care workers may contract the disease at work as they have close and frequent contacts with sources of tuberculosis. However, the number of confirmed cases of tuberculosis in health care workers was pretty low before 1997. The number increased drastically in 1998 and 1999. The increase was mainly due to the enactment of the Occupational Safety and Health Ordinance in 1997 when tuberculosis in health care workers was added to the list of notifiable occupational diseases. The duty to notify was further promulgated by the distribution of the "Guidance Notes on the Diagnosis of Notifiable Occupational Diseases" to all medical practitioners in the medical registry. This might be the reason for the increasing awareness of doctors to notify the disease rather than a genuine increase in the number of cases. Over 90% of the patients worked in public hospitals and clinics. The rest worked in homes for the elderly, private clinics, and other health care services. This includes de Quervain's disease, trigger fingers, tenosynovitis at wrist, tennis and golfer's elbow related to repetitive movement of the hand or wrist. Among all the confirmed cases in the past five years, around one-third of the patients worked as manual labourers in construction sites and factories, and the other one-third worked in the service sector such as catering, hotel and retail industries. Another one-fifth worked in offices and most of them were typists, clerical staff and secretaries. The rest came from various sectors including health care workers. There is no obvious trend of the occurrence of tenosynovitis cases. However, it is expected that more cases will be notified in the coming years due to the increased awareness of such diseases by the general public as well as medical professionals. Occupational skin disease is reported to be the commonest occupational health disorder in many countries. In the United States, it accounted for more than 45% of reported work-related diseases in the 1970s and 1980s.4 In Sweden, it accounted for about 50% of all registered occupational diseases. Recently, statistics collected by the United States Department of Labour indicate a drop in frequency to approximately 34%.5 The true incidence should be many times higher than the reported figures. The reasons may be due to underreporting, under-recognition and limited disability caused by the skin condition allowing affected workers to continue working. Occupational dermatitis is classified into two main types: irritant contact dermatitis, which is more common, and allergic contact dermatitis, which can be diagnosed by patch test. The number of confirmed cases of occupational dermatitis is quite stable and ranged from 18 cases to 34 cases per year. The causative agents identified were detergents, shampoo and hair dyes, organic solvents, cement, rubber gloves, food additives, engine oil and other industrial chemicals. Role of family physicians A significant proportion of patients attending family physicians come from the work force. Work-related illnesses amount to 32% of people interviewed in a survey conducted in 1997-98.6 It is important that family physicians should take a full occupational history because the illness may be linked to early occupational exposure particularly for occupational diseases with a long latency period. All family physicians are urged to notify suspected occupational diseases that come to their attention to the Commissioner for Labour. Alternatively, family physicians are welcome to refer patients suffering from suspected work-related health problems to the two occupational health clinics in Kwun Tong and Sham Shui Po run by the Occupational Health Service of the Labour Department. Patients referred to the Occupational Health Clinics will also be thoroughly investigated. The notification of an occupational disease will initiate a chain of events often including the investigation of the index cases and active searching of other workers to identify other cases. Recommendation of specific preventive measures will be given and follow up evaluation of the effectiveness of preventive measures will be conducted at the workplace in due course. Feedback on our investigation will be given to the referring family physician to facilitate the subsequent follow-up management of patients. Any enquiries about the Occupational Health Service can be directed to the telephone number 2852 4041 or via e-mail to laboureq@labour.gcn.gov.hk Key messages
M Y Ho, MBChB, MMed(OM), FHKCCM
Senior Occupational Health Officer, W K Lo, MBBS, MSc(OM), FAFOM RACP, FHKAM(Community Medicine) Occupational Health Consultant, Labour Department, HKSAR. Correspondence to : Dr M Y Ho, Labour Department, 15/F Harbour Building, 38 Pier Road, Central, Hong Kong.
References
|
|