|
March 2001, Volume 23, No. 3
|
Discussion Paper
|
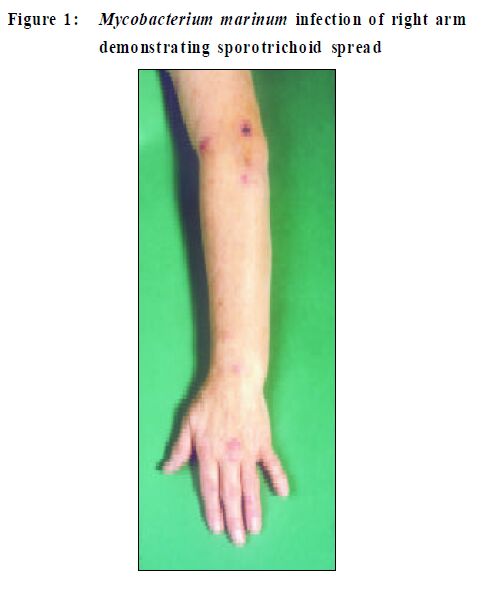
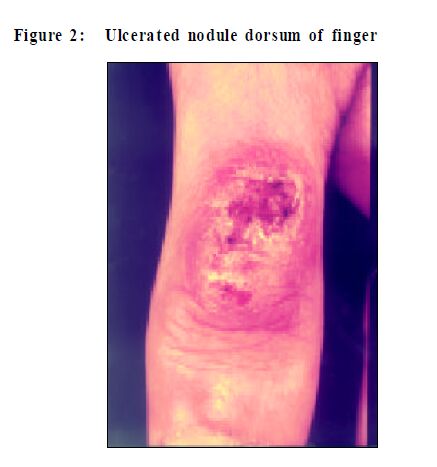
Mycobacterium marinum infectionsVBlackwell, RYu Summary Mycobacter ium mar inum is a saprophytic atypical mycobacter ia capable of causing soft tissue infections in humans, generally acquired via inoculation. M.marinum resides in aquatic environments both fresh and salt water and has a worldwide distribution. The commonest source of infection presently, however , is from a home aquarium and the disease is known as "Fish Tank Granuloma". The typical clinical features are of a nodule, which may be warty or ulcerated, predominantly on the upper limbs. Sporotrichoid spread where further nodules develop adjacent to the initial infection via lymphatic spread is characteristic. M.marinum, similarly to other atypical mycobacteria, is resistant to standard anti-tuberculous therapy. Various treatment regimens have been reported to be effective including rifampicin, co-trimoxazole and tetracyclines. Introduction Mycobacterium marinummaycause opportunisticskin and soft tissue infections in humans. Infection is usually acquired via inoculation in an aquatic environment and the commonest source is the home aquarium. Aetiology Mycobacterium marinum is an atypical mycobacteria which was first recognised as a fish pathogen1 and may also rarely cause disease inman. It is a saprophyte that resides in aquatic environments, both fresh water and marine with a worldwide distribution. In man M.marinuminfections are acquired by inoculation intothe skin in such environments. M. marinum is a member of the slow growing group of mycobacteria and may take several weeks to grow when cultured fromclinicalspecimens. Ithasparticular temperature requirements for growth and will produce colonies on Lowenstein Jensenmedia if grown at 31-33°C, but growth maybe inhibited if culturedat 37°C. Itwill produce ayellow/ orange pigmenton exposure tolightand is thereforetermed a photochromogen. Epidemiology Initial reports of human infectionwere associatedwith swimming poolswhereskin abrasionssustainedfromthewalls ofopenairswimming poolsfacilitatedentryof theorganisms.2 Lesionsassociatedwithswimmingpools are nowless frequent because of improvedconstruction and chlorination. Recently the source of infection reported from many countries is increasingly a home aquarium and the disease is known as aquaristdisease or fish-tank granuloma.3-6 Infectionisusually acquiredwhilst cleaningout the tank andthe patientmay give a history of some of the fish dyingpreviously. It is also noted in peoplewho handle seafood such as fishermen.7 Sincethe HIV epidemic and the increased number of patients undergoing organ transplantation, a number of infections associated with immunosuppression have been reported.8,9 Person to person transmission does not occur. The annual reported incidence of M.marinuminfection is variable; between 0.05-27/100000members of the adult population in North Carolina were reported having the infection.6 In the United Kingdom from 1993 to 1997 an averageof 14.5 casesperannum were reported (Information supplied by PHLS Communicable DiseasesCentre, United Kingdom) but this isprobably an under representation of the actual number of casesoccurring in the UKeach year. Clinical features The incubation period varies from 4-8 weeks5,6 and as the infection is acquired through inoculation the lesions are sited predominantly on theupper limbs. In aquariumkeepers inoculation sites commonly affect the dorsal surfacesof the metacarpophalangeal and interphalangeal joints of the dominant hand. In those cases associated with swimming pools the frequently abraded areas such as the knees and elbows are also affected.2 Typicalclinical features are nodules, whichmay ulcerate. Sporotrichoid spread of the infection is also characteristic of M.marinuminfections although itmay also occur in other infections such as sporotrichosis, nocardiosis, leishmaniasis and other mycobacterial infections.10 Disseminated lesions are less frequently seen buthavebeenreported in achildwhosebathwasusedto clean the family fish tank.11 More rarely disseminated skin lesions have been reportedinimmunocompromisedindividuals8,9,12,13 andsuchpatientsmay also have visceral involvement.13,14 The individual lesions may be verrucous and clinically may resemble tuberculosisverrucosa cutisorothermycobacterial infection, sporotrichosis, Nocardia infection,syphilisor skin tumours. Regional lymph nodesmay be enlarged but do not break down,unlike scrofuloderma. Atypical case is shown in Figures 1 and2.Althoughmost commonlyassociatedwith skin infection M. marinum hasbeen frequently reported as causing arthritis and tenosynovitis particularly of the hand and wrist.15,16 Such lesions are again theresult of penetrating trauma, in particular from fish spines or bones, bites from fish or crabs or injuries whilst repairing fishing equipment. Intheimmunocompetent patientthe lesions tend toeventually heal spontaneously after some months,6 although thismay extend to several years in some cases.17,18
Investigations The diagnosis of cutaneous mycobacterial infections, including those caused by M.marinum can be problematic. Itrelies on the combination of (a) the identificationofvarious clinical features (b) an appreciation of thehistoryof exposure (c) the demonstration ofmycobacteria within the tissue and (d) culture of the causative organismin appropriatemedia. The clinical featuresof ulcerated or warty nodules give rise to abroad differential diagnosis includingM. tuberculosis infection, syphilis, deep fungal infections, foreign body granulomata and occasionally epidermal tumours and therefore adequate investigation of the patient must be undertakento exclude these alternativediagnoses evenwhen the diagnosis of M. marinum infection is suspected. A skin biopsy isgenerally required forhistologicalexaminationand special stains formicro-organisms (Zeehl-Neilsen stain for Mycobacteria,Wade- Fite stains for leprosy,PAS stain for fungi) and polarisation for foreign bodies. The organisms may be cultured from swabs taken from the lesion or skin biopsymaterial. It isimportanttoaskthelaboratory to perform additional low temperature culture if M. marinumor other atypicalmycobacterial infection is suspected. Inthe case ofM.marinuminfections ahistory ofexposure to water, tropical aquaria or fish and in particular trauma in anaquatic environmentmaybea strong clueto the underlying diagnosis. Ingeneral,thehistological featuresof the cutaneous mycobacterioses varywidely and tend not to correlate well withany particular species ofmycobacteria.19,20 Similarly, in M. marinum infections a range of histological featuresmay beobserved fromacutedermalinflammationwith neutrophils and abscess formation to chronic inflammation with tuberculoid granuloma formation.19 The lesions show hyperkeratosis and pseudoepithelial hyperplasia of the epidermis. Whilst these features are not specific they may helpto narrow the broad clinical differential diagnosis.Acid fastbacilli are rarelyseen.6,19,21 More recentlythe application ofDNAtechnology hasenabledmycobacteriato be identified rapidly and accurately but detection of mycobacterialDNA in skin biopsy specimens is only recently becoming widely available.21,22 Treatment As infection with M. marinum is relatively rare there havenotbeenany large clinicaltrialstodeterminethe optimum treatment regimenor relative response ratesto variousdrugs. In common with other atypical mycobacterial infections M. marinumis resistantto standard anti-tuberculous therapy. Antibiotic regimenshave variedbut fall into three categories: rifampicinusuallywithethambutol,co-trimoxazoleandfinally tetracyclines (in particularminocycline and doxycycline). A number of casereports and small studieshave reportedthese drugs being used alone or in combination to be effective in the treatment of M. marinum infections.6,17,23,24 Whilst minocyclineis oftenusedas first linetherapytreatmentfailures havebeen reportedand rifampicinwasused successfully as a single agent in four cases who did not respond to minocycline.6,24 Newer macrolide antibiotics, such as azthromycin and clarithromycin have also been shown to be useful in the treatment of cutaneousM. marinuminfection; clarithromycinmay be used in combination with rifabutin.25 The optimumlengthof treatment has alsonotbeen determined. Forexample, Huminer etal5 recordsan average of 16weeks' therapy whilst Edelstein suggests 1-2 months following resolution of the lesions.6 Small, solitary lesions may be amenable toexcisionorablative treatmentsuch ascryotherapy. Conclusion Aquariumenthusiasts are not always aware of the risks of infectionassociated with their hobby and therefore public education of the riskand simple preventivemeasures such as wearing gloves to clean the tanks, especially if patients are immunocompromised,may be very useful. Cliniciansneed to take careful histories for exposure in patients with such lesionsand informthe laboratory if M. marinuminfection is suspected, so that the appropriate culture conditions can be instituted. Key messages
V Blackwell, BMBS,MRCP(UK), MD
Specialist Registrar in Dermatology, R Yu, MA, FRCP, MD Consultant Dermatologist, Depar tment of Dermatology, Middlesex Hospital, University College London Hospitals Tr ust. Correspondence to : Dr V Blac kwell, Depar tment of Dermatology, Middlesex Hospital, Mor timer Str eet, London. W1N 8AA.
References
|
|