|
June 2001, Volume 23, No. 6
|
Update Articles
|
The interesting phenomena of delusional disordersK Y Mak 麥基恩 HK Pract 2001;23:251-257 Summary Delusional disorders are not uncommon psychotic disorders, yet they are not readily recognised by doctors. There are different types of delusional disorder, some of which are centered on issues of love, hate, obsession, persecution or physical illness. These patients sometimes present to non-psychiatrists and have no insight into their problems. Occasionally, aggressive acting out behaviour, including homicide and suicide, can be frightening. Although treatment is difficult, many do respond well to anti-psychotic medications. 摘要 妄想症並非是一種罕見的精神疾病,卻不容易為 醫生所識別。妄想性疾病的種類繁多,可以表現為 愛、恨、強迫、迫害和軀體疾病。病人無自知力,但 會看非精神病科的醫生。偶而也可能出現令人震驚的 侵犯性表現(例如殺人或自殺)。妄想症的治療並不 容易,但許多病人對抗精神病藥物反應良好。 Introduction A delusion is defined as a false, fixed and unshakable belief that is out of keeping with the patient's social and cultural background; it can be either bizarre or nonbizarre. The delusion in delusional disorders is nonbizarre, meaning that the belief is possible albeit highly unlikely. Nevertheless, the demarcation between bizarre and non-bizarre is becoming indistinct. In his comprehensive book on this disorder, Munro advocated that typical paranoid schizophrenia (with its characteristic bizarre delusions) should be included as a delusional disorder.1 Delusional disorders were previously known as paranoia (and were quite often included as part of the diagnosis of schizophrenia). Paranoia literally means delusional, but many English-speaking psychiatrists use it to refer primarily to delusions of persecution.2 The term implies a habitual attitude of distrust, suspiciousness and irritability in an individual. Delusional disorders were only revived by the DSMIIIR in 1987 to denote a particular group of psychotic conditions with distinct characteristics. In recent years, two other syndromes – paraphrenia and delusional misidentification syndromes – have been added to this category. The onset of delusional disorders may be insidious but occasionally they develop acutely. Some patients keep their delusions secret for long periods of time, and may even hide them behind religious or political activities. Occasionally, they collide with the authorities or the social norms. It is of interest that many patients can change from delusional to normal modes of thought and behaviour easily,3 at least temporarily, and thus succeed in deceiving others. Etiology Little is known about the etiology of delusional disorders. The following are some theories of possible causes:
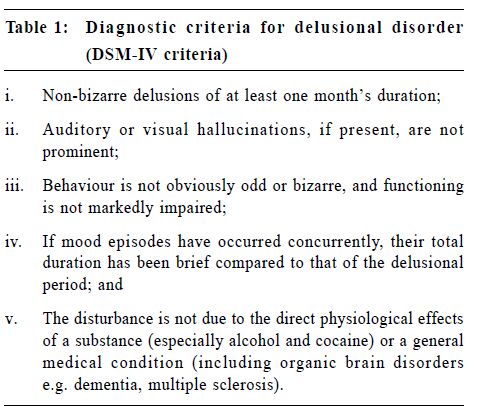
Freud6 emphasised libidinal processes, proposing that paranoia was a regression from the homosexual phase to a fixation at the primary narcissistic phase. Forbidden homosexual love is projected into suspiciousness and rejection. Other analysts also postulated homosexual love, narcissism and projection defenses as causes for delusional disorders. Sullivan7 suggested that delusions might overcome feelings of inferiority and weakness; the delusional state might then be a more comfortable state than tortured sanity. Aronson8 believed that the patient was living in a state of continually threatened autonomy. Epidemiology Although seemingly uncommon in the medical setting, delusional disorders are not really rare. Many cases, of varying degrees of severity, go unrecognised in the community. Primary care doctors are often the point of first medical contact and psychiatrists are the last professionals who see and treat these patients. The familial risk is unknown, but the total incident rate is 1 to 3 cases per 100,000 population. The overall prevalent rate is higher, around 3 per 10,000, and in fact is probably even higher as many cases are undiagnosed. Females and males appear to be equally affected, and the age range is very wide (from the 20s to the 90s with an average of about 40 years of age).1 Many patients are single (unmarried, divorced or separated), and many of those who are married did so before they developed the disorder. The premorbid personality is said to be isolated and asocial (Cluster A personality disorders). It has been said that deafness is associated with late paraphrenia, but a good comparison group is lacking. So far, blindness has not been associated with delusional disorder. Classification According to the DSM-IV and the ICD-10, delusional disorder is one disorder with various sub-types (Table 1).
There are a number of interesting sub-types, including:
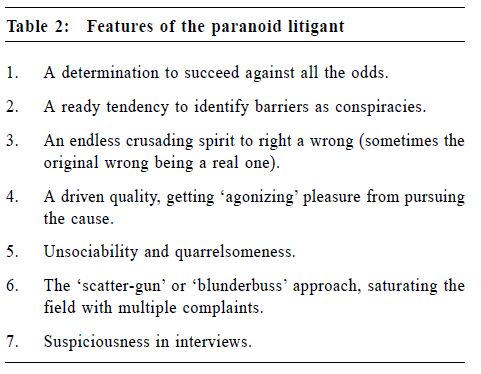
These patients have a fixed belief of being persecuted or harmed. As one would expect, persecutory delusions tend to make the patient extremely wary and guarded, and frequently other related persons are incorporated into the delusional system.1 Particular forms include querulous delusions (also known as litigious paranoia) and reformist delusions (religious, political or philosophical delusions against society). In the former case, there is a strong sense of being wronged (real or imagined wrongs, by other individuals or by the authorities) and a belief that there should be redress through the legal system. The patient may engage in prolonged or repeated litigation. Although the majority of patients are men,d'Orban reported on a group of women in the U.K. sent to prison for contempt of court, many of whom were suffering from a paranoid disorder.9 Freckelton discussed a number of features of such persons for early recognition (Table 2).10 Such patients often dismiss their own lawyers and conduct their own cases. They refuse to pay their fees and threaten to complain to higher levels, sometimes losing sight of the original issue. Many of these patients remain functional, undiagnosed and untreated, until acting out behaviour brings them into the open or into conflict with the legal system. The famous legal case of David McNaghten (who murdered the then prime minister of U.K. in 1843) led to the verdict of 'guilty but insane'. In recent years, the Tarasoff case, in which a deluded Poddar told his therapist of his intention to murder, brought into question the absolute confidentiality of the doctor-patient relationship.
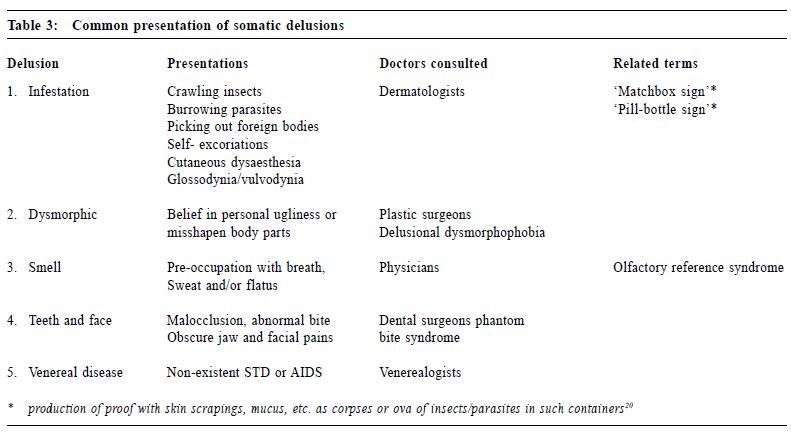
This type is also known as the Othello syndrome,11 which is a pathological or morbid delusion that the sexual partner is unfaithful. The relationship can be homosexual or heterosexual. In many cases, the accusation is totally untrue, but occasionally the partner has actually been unfaithful. This form is regarded as most alarming and dangerous. It is generally focused on one particular person and the patient usually has premorbid traits of jealousy, overpossessiveness and suspiciousness.12 Verbal aggression may escalate into physical violence and end in homicidal and suicidal behaviour. The patient typically spends a lot of time searching for 'proof' of the infidelity and may repeatedly interrogate the partner. Interestingly, the patient will not employ methods that could provide unequivocal evidence of guilt, such as the use of a private detective or videotaping. The condition if untreated can be life long, but sometimes it will disappear when the accused partner is no longer available. The accused partner is often severely distressed, avoiding all social interactions with others. Quite often, it is the partner who asks for help, but occasionally the partner is being brainwashed that he/she is indeed guilty of infidelity.1 Another name for this type of delusional disorder is de Clerambault's syndrome,13 which is a delusion that another person is in love with the individual. It occurs more often in women (Old Maid's Insanity14), but can occur also in men.15 The imagined lover is usually unattainable because of celebrity or marital status, can be homo- or heterosexual, and sometimes may be a 'phantom' that does not really exist.16 The patient is convinced that the other person initiated the relationship, although there has been little or no actual contact between the two. In fact, the patient will avoid the chance of actual contact, and the love letters or presents usually remain unsent.1 If indeed there is contact and the inevitable rejection occurs, the patient usually makes excuses for their beloved, but occasionally there is angry acting-out behaviour, including stalking, harassment, assault, kidnapping and murder. The most famous case is that of John Hinckley Jr., who attempted to assassinate former US President Ronald Reagan in order to attract the attention of a famous female film star towards whom he had erotic delusional feelings.17 Gestures by the other person are often misinterpreted as evidence of passion; rarely there is even an incubus syndrome, which is a feeling (tactile hallucinations perhaps) that there are sexual visits during the night.18 These patients are convinced that they have some physical defect or medical condition and go to extraordinary lengths in physician shopping and treatment. The variety of presentations can be seen in Table 3 below. In a way this represents hypochondriasis of a delusional degree. Lack of therapeutic success does not deter patients from seeking further medical attention. Some report that they smell, see or feel an abnormality and they try various means to get well (e.g. excessive cleaning to remove parasites). Unsuspecting doctors and specialists may prescribe unnecessary medications and perform surgeries that do not work. Patients may also initiate their own idiosyncratic forms of treatment, sometimes of a bizarre and alarming nature. In the long term, many feel angry, abandoned and despairing, with suicidal thoughts and attempts. Synonyms for this type of delusional disorder include monosymptomatic hypochondriacal delusion and the Ekbom's syndrome (presenile infestation delusion).19
These patients have a deluded inflated appraisal (also called megalomania) of their worth, power, knowledge, identity, or special relationship to a deity or famous person. While not very frequently described in the scientific literature, history seems to have produced a number of prominent political figures who may have had such delusions, including Adolph Hitler, President Idi Amin of Uganda and perhaps Henry IV. Patients may adopt a lifestyle that fits in with the delusion, displaying extravagance, marked arrogance, extreme religiosity, etc.Occasionally, a deluded grandiose patient reacts to stress with anger and antisocial behaviour. The Jonestown massacre of 1000 followers of a cult led by Reverend Bob Jones and the mass killing of the Waco congregation were possibly related to such personalities.1 Delusions characteristic of more than one of the above types but no one of them predominates; e.g. delusions of reference without malevolent content. Cotard's syndrome is an extreme kind of nihilistic delusion (delire de negation); for example, the patient might complain that his brain was completely destroyed, or that his family members have ceased to exist. Because of such delusions, social relationships are usually strained, and many such people live in isolation. Delusions of reference may also occur, as may alcohol or drug abuse. These patients tend to be disappointed in the doctors they have consulted, but are angry and skeptical if referred for psychiatric treatment. Related psychotic disorders
This disorder is characterised by the additional presence of auditory hallucinations lasting at least six months, but none of the following: disorganized speech, disorganized/catatonic behaviour, or flat/inappropriate affect.
When two or more persons share the same delusion(s), this is called shared psychotic disorder in the DSM-IV and 'induced delusional disorder' in the ICD-10. There is often a strong emotional link between the persons, usually members of the same family who live together closely but often in isolation from the outside world. One person has a genuine delusion (the inducer or the primary patient), while the delusion in the other person (the recipient) often disappears when the two are separated. This sort of transmission from one to another is called folie imposse.21 It is better to treat the primary patient, however occasionally both persons develop the delusions simultaneously (folie simultanee) and require treatment together. Shared psychotic disorder can occur in more than two persons (e.g. folie a trois) and can even develop within a cult setting, where it is called a 'paranoid pseudocommunity'. It is a rather uncommon phenomenon, but runs a chronic course; and is more frequent in women than men. This is often diagnosed as schizophrenia. Organic causes must be ruled out. Again, there are different forms:
There is a close time relationship between the psychosis and substance abuse or withdrawal; the psychosis then clears. In some, there are persisting symptoms occurring even after consciousness has cleared. Prominent thought disorder is not evident, and dysphoria is not uncommon. There is usually a degree of avolition, sometimes with irritability and ideas of reference. Other differential diagnosis The following disorders may resemble delusional disorder.
At some time there is a mood episode (depressive and/or manic) concurrent with schizophrenic symptoms, but during the illness there have been delusions or hallucinations for at least two weeks in the absence of prominent mood symptoms. A type of personality disorder characterised by eccentric behaviour and anomalies of thinking and affect. There is no definite onset and it resembles schizophrenia, though no definite schizophrenic anomalies occur at any stage. A disorder with schizophrenic symptoms and a manic-depressive course. Some episodes may be precipitated by stress. A form of somatoform disorder in which the patient is preoccupied with an imagined defect in appearance. Management Some of these patients are notorious for seeking psychiatric help, but compliance with treatment is poor. Conducting a search for any underlying medical condition (including substance abuse) is helpful. It is often necessary to assess dangerousness immediately, as homicide and suicide may occur, especially with morbid jealousy.
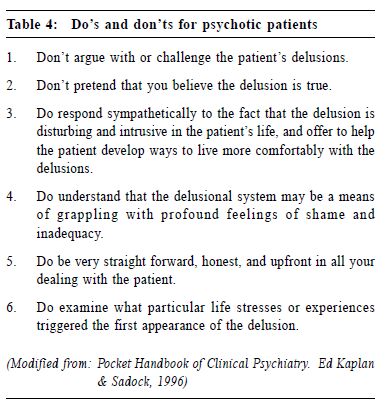
Medications are the mainstay of treatment, (although different types of delusional disorder may merit some specific attention).2 Neuroleptics have been the treatment of choice; pimozide, usually in a low dose, has been found to be particularly useful for the somatic type,27 but the response rate with other types is also quite satisfactory,28 with an overall response rate of 80%. Since pimozide has calcium channel blocking properties at high dosage, it should be used with caution in cardiac patients. Long-acting intramuscular injections may be considered if the compliance with treatment is not satisfactory. If mood symptoms are prominent, including the occurrence of post-psychotic depression, then antidepressants (especially the newer types) are useful. That may be why the atypical neuroleptics are often better than conventional ones. Nevertheless, there are some patients who show no response to drug treatment despite high dosage. Under such circumstances, benzodiazepines and anticonvulsants are worth trying, especially if there is a history of head injury or suspected seizure activity. The goal is to provide support while attempting to change certain behaviours. It is advisable to avoid undue stress including significant life-events. There is evidence that cognitive-behavioural therapy may be capable of modifying the delusions,29 but so far it is mainly an adjunctive treatment rather than a curative measure for the disorder. Psychoanalytic psychotherapy may be too stimulating and harmful. For the caregivers and relatives, there are some suggestions given in Table 4 below. It may be useful to engage family members in the management plan (with the patient's permission). In case of imminent danger, separation from the potential victims by compulsory hospitalisation may be necessary, and it may be necessary to warn the potential victims.
Outcome The prognosis of delusional disorder is varied. Some remit spontaneously, while others are refractory and persist for life. If untreated, many patients can still function at a high level in the community; in other cases, the disorder is disabling and serious. The incidence of violent acts appears to be higher than in the general population, especially in the case of erotomania. Patients have a shorter life expectancy than non-patients because of increased suicide rates and increased risk of death from various other causes (including institutional care and of poverty). Patients with somatic delusions will indulge in very costly investigations and inappropriate treatments, while those with persecutory delusions may cause social disruption and perhaps political fanaticism. Perhaps one day, another paranoid figure like Hitler may arise. Conclusion Delusional disorder is a disorder in its own right, and is more common than previously thought. Patients are often seen not by psychiatrists, but by dermatologists, infectious disease specialists, cosmetic surgeons and general practitioners. There is still confusion about the inclusion or exclusion of various syndromes; more research will clarify this in the future. Key messages
K Y Mak, MBBS, MD, DPM, FRCPsych
Clinical Associate Professor (Part-time), Department of Psychiatry, The University of Hong Kong. Correspondence to : Dr K Y Mak, Department of Psychiatry, The University of Hong Kong, Queen Mary Hospital, Pokfulam Road, Hong Kong.
References
|
|