|
July 2001, Volume 23, No. 7
|
Update Article
|
Surgical management of a drooling childK C Tang 鄧廣智, Y Hui 許由, W H S Goh 吳慧雪, R To 杜偉業, W I Wei 韋霖 HK Pract 2001;23:285-289 Summary Drooling is a physiological process in infants. When it persists beyond the age of 4 years, it becomes a clinical symptom. Drooling is a common problem among children of all ages with a neurological deficit. It causes significant decrease in the quality of life of the children and their families. Parents often accept the disability because they are not aware that treatment is available. Doctors should recognise the problem during a consultation and discuss the available management options. Patients should be referred to a drooling clinic that adopts a multi-disciplinary approach. Management of drooling has been evolving over the last thirty years. Surgery has become a safe and effective management option. 摘要 流涎是嬰兒的正常生理現象。但如果持續到四歲 以上時,則成為病徵。對於患有神經系統疾病的兒童 來說,涎漏是一個普遍的問題。它影響病人及其家屬 的日常生活。因為家長不知道此症可以治療。唯有接 受現實。醫生在診治時,若發現此情形應與病人家屬 討論各種不同的治療方式。病人應當被轉介至專治涎 漏的專科。涎漏的診治於過去三十年不斷發展,外科 手術是其中一種安全而有效的方法。 Introduction Drooling, or sialorrhoea, is defined as spillage of saliva from the mouth. It usually causes much physical and psychological distress to the patients as well as their families. Saliva overflow may cause peri-oral maceration, chapping and infection as well as soiling of clothes, carpets, toys and books. In addition, it causes social embarrassment leading to impairment of education and development. This is particularly significant when a child possesses normal intelligence. Family members are also affected. They may avoid going out with a drooling child because of social stigmatisation. In addition, the frequent need to change soiled clothes is distressing and can affect the relationship between the care provider and the child. Drooling is not a life-threatening condition and thus a problem that is often overlooked by the health-care provider. As the traditional Chinese culture stresses on endurance, parents of a drooling child often do not highlight the problem to doctors. Family physicians are in a good position to raise the issue, and to inform the parents of the different treatments available. Successful control of drooling improves appearance, hygiene and selfesteem of the patient. It reduces the work of the caretakers and improves the quality of life of the child and their family members. Classification Drooling can be classified as physiological, acute or chronic.1 Normal infants drool and this usually stops by the age of 18 to 24 months. However, intermittent drooling up to the age of 4 years may occur in children with no neurological deficit.2 Many acute inflammatory conditions, such as acute epiglottitis and acute tonsillitis may also cause drooling because of odynophagia. This usually improves as the inflammation subsides. Most patients with chronic drooling usually have various forms of congenital or acquired muscle spasticity or incoordination. They may also be mentally disabled due to other co-existing medical problems. It is estimated that 10% of children with cerebral palsy suffer from drooling.3 Long-term use of tranquillizers or anticonvulsants might also worsen the problem because of their cholinergic action. Pathophysiology Approximately 1.5 litres of saliva is secreted each day. Most of the secretion is produced by the major salivary glands in the following ratios: Parotid (25%); submandibular (70%); and sublingual (5%).2 Most of the resting saliva secretion is produced by the latter two glands, which contain higher levels of glycoproteins and is thus more viscid. Hence the clinical troublesome symptoms of drooling are caused mainly by secretion from the submandibular glands. Pathological drooling is due to either hypersecretion of saliva or neuromuscular dysfunction of swallowing.4 Hypersecretion as a cause of drooling is less common. It may be seen in children with gingivitis, rabies, mercury poisoning or after anticholinesterase ingestion.5 The act of swallowing has four distinct but continuous phases:
This is a highly complex act with coordinated muscle movements involving the lips, tongue, palate, jaw, pharynx, larynx, oesophagus and respiratory muscles.3 Drooling in general results from defect in the oral phase of rather than the pharyngeal phase of swallowing. Clinical Assessment A multidisciplinary team approach is essential in the evaluation and management of a drooling patient.6,7 The team usually consists of a paediatric otorhinolaryngologist, speech therapist, paediatric neurologist and paediatric dentist. Speech therapists give assessment depending on the severity and frequency of drooling. Previous attempts at non-surgical treatment should be documented. Oral motor function is also assessed and the possible outcome of further non-surgical treatment is estimated. An oral motor habilitation programme should be conducted before surgical management is recommended. The paediatric dentist provides information on the status of the dentition and occlusion. The condition of the teeth and gums, and the configuration of the mandible and palate are assessed. The paediatric otorhinolaryngologist will also assess the position and control of head movements, the nature of the drooled saliva, tongue size and mobility, as well as a thorough head and neck examination. The impact of drooling on the child, parents and other family members is assessed. Management options are explained with respect to the predicted success rate and potential complications. Management No treatment Children under 4 years of age who have occasional mild to moderate drooling should be observed. Patients with chronic aspiration or severe global developmental delay are not candidates for surgical intervention because drooling is usually one of the least worrisome problems in these patients. Oral motor programmes Oral motor training aims at improving:
It is non-invasive and, occasionally, children may benefit from this type of therapy alone. It has been shown that 75% of children who received the oral motor habilitation programme for 6 months demonstrated improvement in both the visual analogue scale and Drooling Quotient.11 It is generally recommended that children over the age of 6 years should receive at least 6 months of training before other methods are considered. However, despite some improvement in most children, oral motor programmes are unlikely to eliminate the drooling problem entirely.10 Correction of situational factors Some situational factors may contribute to drooling. For example, poor sitting posture with the head tilted forward encourages sialorrhoea. Therefore, the correct sitting posture should be taught to the caregiver. Nasal obstruction causes open mouth breathing and aggravates drooling. Pharmacological treatment can usually control nasal obstruction. If there is gross nasal septal deviation or turbinate hypertrophy that is unresponsive to medication, surgical correction can be offered. Dental disease will also cause drooling. For example, mal-occlusion is common among patients with cerebral palsy. Sometimes, corrective orthodontia and even orthognathic operation is necessary. Anticonvulsants may cause sialorrhoea, and therefore a neurologist’s opinion is required to determine whether an appropriate alternative therapeutic agent can be given. Nevertheless, even when all these factors have been corrected, only 10% of patients show significant improvement.7 Biofeedback with behaviour modification In this management modality, a sound stimulus is usually employed. The therapy aims at conditioning the child to swallow every time a signal is heard. However, this method requires multiple sessions and is very timeconsuming. In addition, the child needs to be of average intelligence and should be old enough (over 8 years of age) to understand the training. Severe drooling does not usually respond to biofeedback. Hence only a small number of patients may benefit.2 Pharmacotherapy Use of medication, such as like transdermal scopolamine is only recommended12 for short-term management. Side effects such as constipation, urinary retention, skin reaction and high cost make long term use of pharmacotherapy difficult. Surgery Surgical management of drooling is performed when the patient cannot benefit from further non-surgical therapy. It is usually performed when the neurological status is stable and the patient is over 6 years of age.2 Operations to treat drooling can be divided into two main types. 1) to decrease saliva production; 2) to redirect salivary flow to facilitate swallowing. Types of surgery
The operation was first described in 1962 by Golding-Wood.13 The operation can be performed permeatally without a visible surgical scar. The chorda tympani which is a branch of facial nerve and the tympanic plexus which is mostly derived from Jacobson’s nerve (a branch of the glossopharyngeal nerve) are divided. Technically, the procedure is relatively simple and has a reported drooling control rate of 74%.14 The disadvantages of the operation include sensory loss of taste and potential damage to hearing. More importantly, drooling often returns to preoperative levels within 6 months. Therefore, this surgery has been superseded by other procedures. This is a simple and safe operation. However, it leaves an external surgical scar on the patient’s neck. In addition, it carries the potential risk of injury to the lingual and hypoglossal nerves as well as to the marginal mandibular branch of the facial nerves. This is also a simple and safe procedure. However, it carries a significant morbidity in terms of tender swelling of the glands, which may be prolonged and difficult to treat.
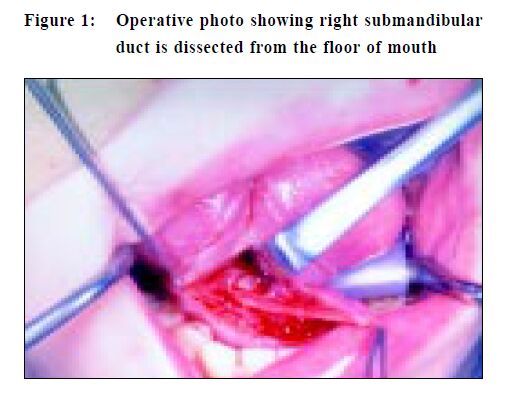
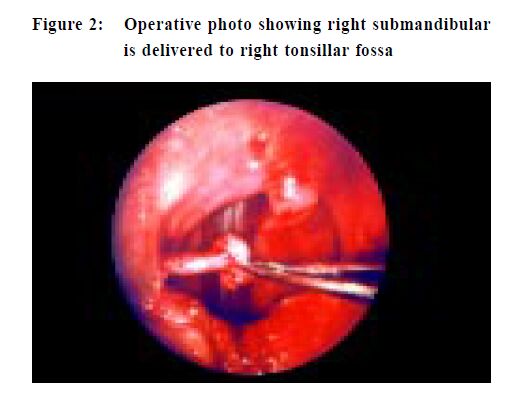
Fistulisation of parotid ducts to the tonsillar fossae was first described by Wilkie.15 The procedure carries a high risk of complications such as duct stenosis, septic parotitis and external surgical scarring. As mentioned earlier, the problem of resting drooling is due to saliva production by the submandibular gland. It is therefore more logical to reroute the submandibular duct. This is one of the most commonly performed surgical procedures for drooling in which consistent control can be expected.16 It was first described in 1974 by Ekedahl.17 The aim of the procedure is to direct the opening of the submandibular ducts from the anterior floor of mouth to the tonsillar fossae. Saliva in the oropharynx triggers the pharyngeal phase of swallowing that is usually intact in most drooling patients. Tonsillectomy is usually performed first to facilitate the placement of the duct. The incision is intraoral and leaves no external surgical scarring. The submandibular duct is dissected from the floor of mouth (Figure 1) and tunneled in a submucosal plane to the tonsillar fossae on the floor of the mouth (Figure 2). As the sublingual gland is closely related to the submandibular duct, damage to it is inevitable. Hence, ranula is a known complication in 10% of patients.18 To avoid this particular complication, some surgeons routinely perform sublingual gland excision.
The control rate of drooling following this procedure is 89%.9 It has been remarked that the operation causes scarring of the duct, which is similarly observed with submandibular duct ligation. However, postoperative technetium scanning showed that physiological function is preserved in at least one of the glands if a bilateral procedure is performed.18 Conclusion Drooling is a common problem among children with a neurological deficit. It causes significant morbidity as well as decreases the quality of life of the children and their families. It is a problem that can be managed by a multi-disciplinary approach. The drooling clinic established in Duchess of Kent Children’s Hospital has around one hundred referrals over the past five years. However, this does not reflect the true incidence as some parents may not be aware of the possible treatment of the problem. Although surgery is more invasive than other treatment options, it is the most effective and allows longterm control of sialorrhoea. As submandibular duct repositioning with sublingual gland excision is simple and effective with low morbidity and complication in expert hands, this is the treatment of choice for a drooling child. Key messages
K C Tang, MBBS(HK), FRCS(Glasg)
Medical & Health Officer, Department of Otorhinolaryngology, Queen Mary Hospital. Y Hui, MBBS(HK), FRCS(Edin), FACS, FHKAM(Otorhinolaryngology) Consultant, W I Wei, MS(HK), FRCS(Edin), FACS, FHKAM(Otorhinolaryngology) Professor of Otorhinolaryngology, Division of Otorhinolaryngology, Department of Surgery, University of Hong Kong Medical Centre. W H S Goh, MBBS(Singapore), MMed(Paed)(Singapore), FRCP(Edin),FHKAM(Paediatric) Consultant, Department of Paediatric, Duchness of Kent Children’s Hospital. R To, BAppSc(Sp Path) Speech Therapist, Department of Speech Therapy, Children’s Habilitation Institute, Duchess of Kent Children’s Hospital. Correspondence to : Dr K C Tang, Department of Otorhinolaryngology, Queen Mary Hospital, Hong Kong.
References
|
|