|
July 2001, Volume 23, No. 7
|
Case Report
|
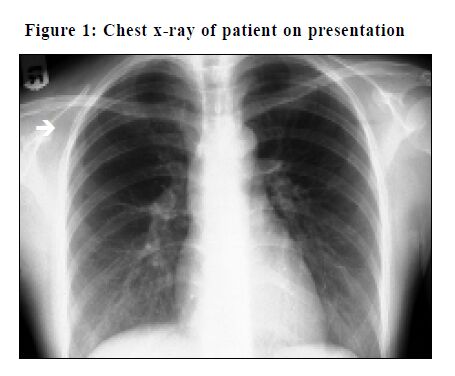
A case of Macleod’s SyndromeN Y Chan 陳迺賢, W Y Chan 陳惠儀, D V K Chao 周偉強 HK Pract 2001;23:301-303 Summary Macleod’s Syndrome is a variant of obliterative bronchiolitis due to an affected hypoplastic lung. The prognosis is good and most patients run an asymptomatic course only to be discovered as an incidental finding on chest radiography. There is no specific treatment for Macleod’s Syndrome. The appropriate thing to do is to reassure the patient with a clear explanation and suggest that the patient avoid or stop smoking to prevent further damage to the lung. 摘要 麥克勞德氏綜合症是肺部發育不全而引起的一種 堵塞性細支氣管炎。大部份患者沒有病徵,因為照 × 光時意外發現。雖然此病尚無特異性治療方法,但 其預後良好。 適當的處理方法是透過詳細的解釋,消除病人的 疑慮,建議病人避免或停止吸煙,以免肺部受到進一步損害。 Clinical information A 21 years old lady attended for a pre-employment check-up. She was a non-smoker and enjoyed good past health. She was asymptomatic at the time of the body check. On physical examination, her general condition was good. She was not cyanotic. The trachea was centrally located. The chest expansion was equal and symmetrical on both sides. There were slightly diminished breath sounds over the right upper zone. There were no rhonchi, nor any crepitations on auscultation. The percussion notes were normal on both sides. The examination of the cardiovascular system, abdomen, and the central nervous systems were normal. A screening radiograph of the chest was performed. Radiological findings The penetration of the chest radiograph was adequate. The film was not rotated. The heart size was normal and the lung fields were clear. There was an area of increased transradiancy seen in the right upper lobe with diminished vascularity. The lung volume was normal. There was no displacement of the mediastinum. The findings were compatible with Macleod’s Syndrome, with segmental involvement. (Figure 1)
Discussion Macleod’s Syndrome is also known as Swyer-James Syndrome. It is considered to be a variant of obliterative bronchiolitis, which is characterised by bronchiolar narrowing or obstruction due to submucosal and peribronchiolar inflammation and fibrosis.1,2 It is probably related to viral infection occurring in infancy or early childhood. The condition is usually unilateral. As the damage occurs during the stage of lung growth, the affected lung becomes hypoplastic. The prevalence of this syndrome is unclear. Most patients are asymptomatic. It is often an incidental radiographic finding in an apparently healthy adult. There is occasionally a history of repeated respiratory tract infections during childhood. A few patients may experience exercise-induced breathlessness.3 On examination there is usually no significant abnormality detected. In some cases, there may be reduced chest expansion and diminished air entry on the affected side.3 The chest radiograph shows increased transradiancy of the whole or part of one lung with diminished hilar and peripheral vascular shadows. Other investigations may help to establish the diagnosis. Lung function tests and spirometric studies may show a mildly obstructive pattern. Lung perfusion scanning may show reduced ventilation and perfusion to the affected lung.3,4 The differential diagnosis of Macleod’s Syndrome would include other causes of hypertransradiant lung. Most of them can be identified by history taking, clinical examination or by other radiographic views of the chest. These causes include:
It may show a rotated thoracic spine on the film. One side of the lung may be apparently larger and more translucent. The sternocostal origin is the most commonly missing part in this condition. The affected side of the chest wall is flatter on inspection, especially in the male patient. The patient may also have weakness of adduction or medial rotation of the shoulder joint. A past history of breast disease with mastectomy, together with a surgical scar on the chest wall may help to clarify the diagnosis. The patient may experience sudden onset of a sharp chest pain, with associated breathlessness. On examination the percussion notes are hyper-resonant and the breath sounds are diminished on the affected side. In tension pneumothorax, the trachea may deviate to the contralateral side. The breath sounds may be significantly diminished. An erect chest radiograph may demonstrate a pleural edge with a clear space beyond it in case of mild pneumothorax, or complete collapse of one lung in that of tension pneumothorax. The patient may experience chest pain, breathlessness, and syncope during the attack. A past history of deep vein thrombosis may suggest the diagnosis. The patient may be in shock and desaturate in severe cases. Electrocardiography may show a classical S1Q3T3 pattern. Lung perfusion scanning and pulmonary angiography may be used to establish the diagnosis. Bronchial obstruction, either complete or partial, due to tumour or foreign body can occasionally produce unilateral hypertransradiancy. On examination, localised rhonchi and diminished breath sounds may be present.3,4 There is no specific treatment for Macleod’s Syndrome. The appropriate thing to do is to reassure the patient with a clear explanation and suggest that the patient avoid or stop smoking to prevent further damage to the lung. Key messages
N Y Chan, MBChB
Medical Officer, W Y Chan, MBChB Medical Officer, D V K Chao, FHKAM(Family Medicine) Family Medicine Cluster Coordinator (KE), Department of Family Medicine, United Christian Hospital. Correspondence to : Dr N Y Chan, HA Staff Clinic, Department of Family Medicine, United Christian Hospital, Kwun Tong, Kowloon, Hong Kong.
References
|
|