
|
September 2019,Volume 41, No.3
|
Original Article
|
A pilot study to assess the awareness of herpes zoster and the attitudes towards herpes zoster vaccination among Chinese patients attending a government general out-patient clinic in Hong KongLong-yee Cheng 鄭朗兒 HK Pract 2019;41:60-65 SummaryObjective: Keywords:Herpes zoster, vaccination, knowledge, acceptance, primary care 摘要目的:帶狀皰疹是一種基層醫療常見的疾病。本調查研究: 關鍵字:帶狀皰疹、疫苗、知識、接受、基層醫療。 IntroductionHerpes zoster (HZ), also known as shingles, is a reactivation of the latent Varicella zoster virus infection in the sensory nerve ganglion. Post herpetic neuralgia (PHN) is a common and severe complication which can persist for months to years.1 There are more than 1 million new cases of HZ in the United States every year and the risk of HZ increases with age.2 The lifetime risk of developing HZ is between 25% and 30%, rising to 50% in those aged over 80 years.15-17 A study analysed the incidence of HZ from 12 countries in Asia-Pacific, Europe, North America and Middle-east. The estimated overall incidence is about 3.4 - 4.82 per 1,000 person-years which increases to over 11 per 1,000 person-years in those aged at least 80 years.17 In 2013, the Public Opinion Programme of The University of Hong Kong conducted a telephone interview about HZ Vaccination targeting Cantonese-speaking local citizens in Hong Kong of age 50 - 80. Out of 2,042 subjects, 344 (16.8%) recalled a previous history of herpes zoster.18 About 10 - 25% of patients infected with HZ virus will have complications such as PHN and HZ ophthalmicus.3 In Asia-Pacific region such as Taiwan and Korea, severe morbidity, and significant healthcare resource utilisation, are also observed to be associated with HZ, supporting the need for preventive strategies to reduce the burden of illness.9,10 The HZ vaccine was licensed in 2006. In 2011, the US Food and Drug Administration approved the use of this vaccine for adults >50 year-old.1 The HZ vaccine reduces the risk of having HZ by 51%.6 It can reduce the burden of illness and the incidence of PHN by 61% and 67% respectively.2,4,6 Although the HZ vaccine is known to be effective to decrease the risk and burden of HZ, vaccination rates have remained low. In 2011, the vaccination rate among adults aged 60 or older was only 15.8% in the US.3 A few studies have assessed the factors associated with and obstacles to HZ vaccination status. Factors that have been found to play a role in influencing patient attitudes towards the vaccine include knowledge on HZ, physician’s recommendation, information from the mass media and history of previous influenza vaccination.1-4 This vaccine was registered in Hong Kong in 2007.7 Currently, there is a lack of information about the awareness and degree of acceptance of the herpes zoster vaccine and the factors influencing patient attitudes towards HZ vaccination in Hong Kong. This study aims to fill this gap in knowledge and to help inform doctors on how their patients can be educated to enhance the HZ vaccine uptake in our setting. MethodsPopulationA convenient sample of patients aged 50 or above was identified and recruited by the principal investigator from a government outpatient clinic in Hong Kong East Cluster between May and July 2016. Patients who were illiterate, who had debilitating psychiatric diseases, or who were in a mental state that was not capable of giving informed consent were excluded. Data collected did not contain protected health information or patient identifiers. The study was approved by the Hong Kong East Cluster Research Ethics Committee. Study design and MeasurementsA structured questionnaire was developed by the principal investigator after taking similar studies on vaccination as references.1, 3-5, 11-14 Some of the questions were adopted from the framework of the Health Belief Model (HBM) about perceived susceptibility, perceived benefits, barriers and cues to action. The HBM has been widely used in different studies to identify patients’ perceptions of disease and vaccination.11-13 Clinic supervisors were invited to check the relevance and comprehensibility of the questionnaire by testing on clinic patients prior to using it on the study subjects. Face-to-face interviews were conducted after the subjects signed the consent form. The interviews took about 10 minutes to complete. Part one of the questionnaire was designed to gather information on the awareness of HZ, knowledge about HZ, previous history of health care provider’s recommendation on HZ vaccination and attitudes towards acceptance of the HZ vaccination. Reasons for or against receiving HZ vaccination were asked depending on the participants’ answers on the acceptance of vaccine. Knowledge about HZ was assessed by asking 6 questions with choices of “Yes”, “No” and “Do not know”. The questions were about the pathology, symptomatology, Chinese myths and complications of HZ. Participants who were not aware of HZ at all were asked to skip the remaining questions of Part one and answer Part two directly. Part two of the questionnaire assessed patient’s sociodemographic factors, history of influenza vaccination in the past two years and personal history of diabetes or cancer. Statistical methodsThe survey data were analysed with IBM SPSS Version 24.0. Chi-square test was used to examine the differences in the effect of demographic factors, knowledge score, past experiences of HZ, past recommendations of HZ vaccination from a health care provider and the acceptance of the HZ vaccine. Univariate logistic regression was used to assess each variable for their associations with attitudes towards HZ vaccination. Multivariate logistic regression was used to examine the attitudes towards HZ vaccination while controlling all sociodemographic factors, knowledge score, recommendation from Health care providers and personal experience on HZ. The cut-off for statistical significance was set at p<0.05. ResultsSample characteristicsA total of 400 Chinese participants aged 50 or above were recruited in the research. None were excluded. Table 1 shows the demographic characteristics and HZ awareness of the respondents. The sample consisted of 185 men (46.2%) and 215 women (53.8%) aged 50 to 89 years (mean age, 65 years). Almost half of the participants (48.5%) were in the 60-69 year-old age group. As the common retirement age in Hong Kong is 60-year-old, 57.2% of the participants reported unemployed and 69.3% of participants were having monthly household income of less than $15,000. With respect to educational level, 52.2% of participants reached secondary school level, and 16% reached tertiary level. As the clinic was located in the Wan Chai district, most of the participants lived on Hong Kong Island (71.2%) and private building (71.2%). 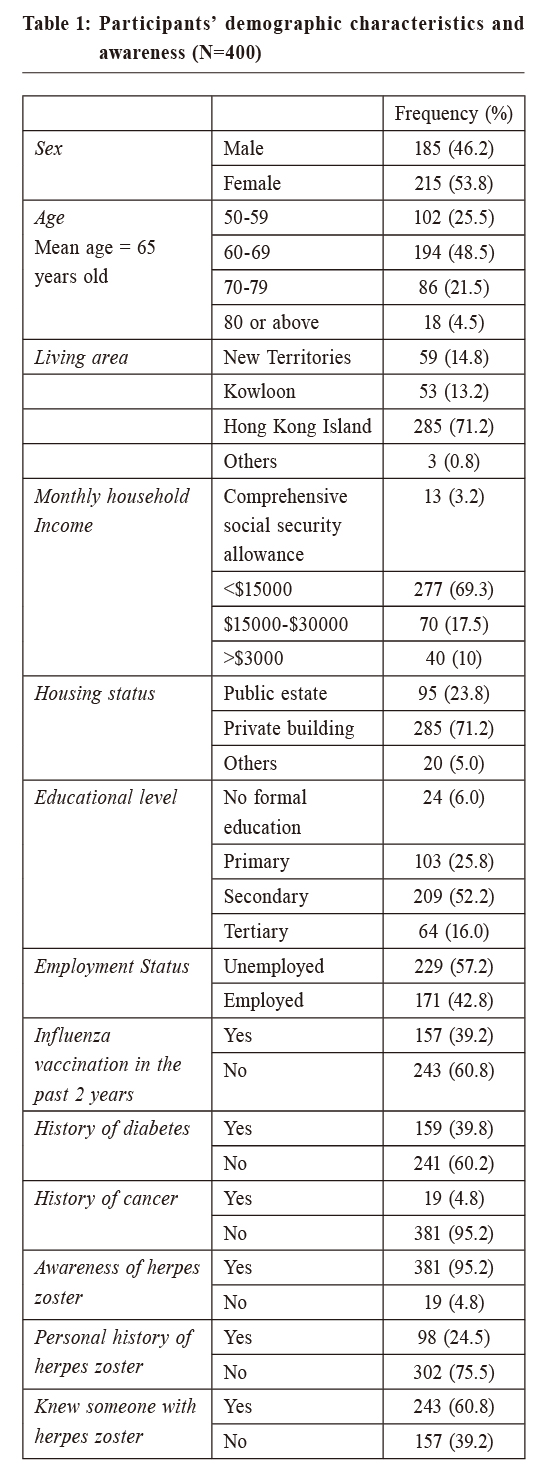
Awareness of HZ Participants were asked if they had ever heard of HZ; 95.2% stated that they were aware of HZ (n=381), 24.5% of the participants had a history of HZ, 60.8% of the participants knew of someone with HZ. Knowledge of HZ and its vaccinationOf the 381 participants who were aware of HZ, their knowledge, acceptance of HZ vaccination and the reason(s) behind their attitude towards HZ vaccination were assessed. In the knowledge test, only 14.4% answered all the six questions correctly (Table 2). Most knew the symptoms of HZ (91.9%), however, there was deficiency in the knowledge on PHN and pathology of HZ. (Figure 1) Only 9.4% had been previously introduced to HZ vaccination by health care providers. 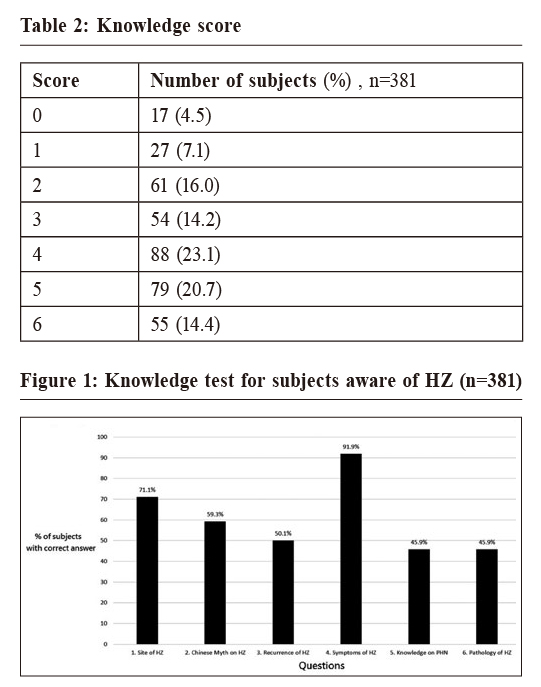 Acceptability of HZ vaccine Among the 381 subjects who were aware of HZ infection, over half of them refused vaccination (54.3%), while 42.5% were agreeable to having the vaccination if asked. Only 12 participants had previously received the vaccination. Univariate logistic regression analysis showed that personal history of HZ, better knowledge on HZ, and history of influenza vaccination in the past 2 years were significantly and positively associated with a willingness to receive the vaccination (Table 3). On multivariate logistic regression , after controlling all demographic factors, knowledge score and HZ awareness variables, only personal history of HZ, and history of influenza vaccination in the past 2 years remained as significant factors. Those with personal history of HZ were 1.76 times more likely to accept vaccination (95% CI, 1.05~2.97) whilst those with history of influenza vaccination in the past 2 years were 2.5 times more likely to receive vaccination for HZ (95% CI, 1.55~4.05). Chronic illness such as diabetes or cancer were not shown to be significantly associated with the acceptance of the vaccine. 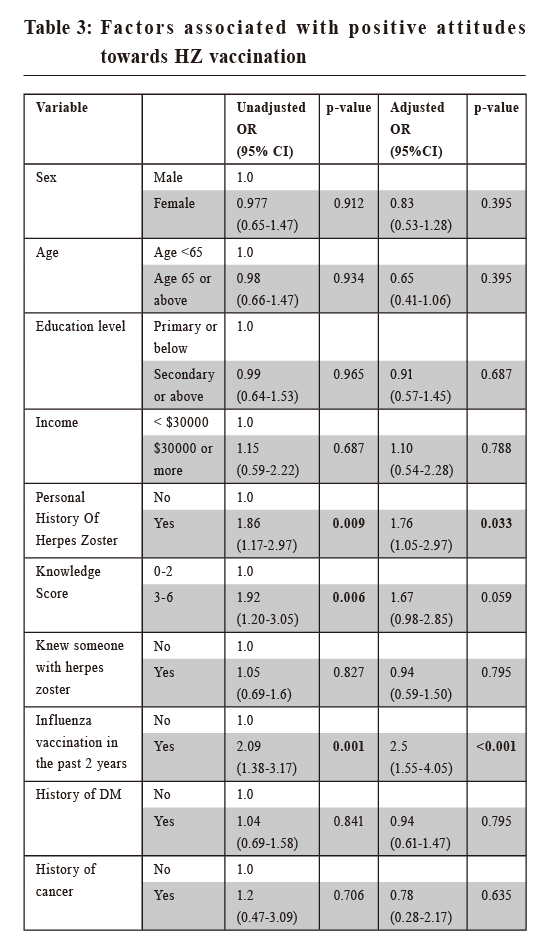 Reasons for acceptanceRespondents who were agreeable to receiving the vaccination were asked why they wanted to have the vaccination (Table 4). The most common answer was “concerned about HZ complications” (84.5%), followed by “Health care provider recommendations” (56.9%), “Reasonable price” (29.3%), “the vaccine is effective” (24.1%), a nd “Family/friends recommendations” (15.5%). A small number of participants responded with “Commercial advertisement” (9.2%). 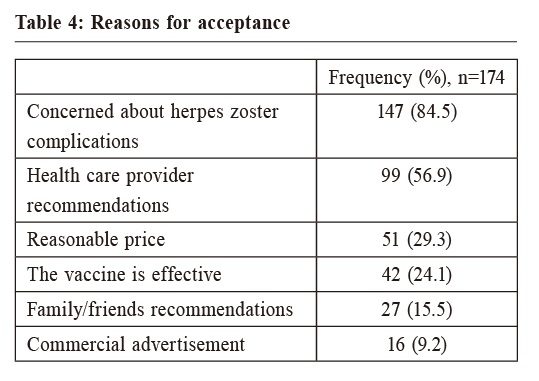
Reasons for refusal of vaccinationThe most common reason underlying a refusal to the vaccination was “No perceived risk of getting herpes zoster” (51.7%), followed by “Afraid of vaccine side effect” (50.7%), “Doubt on vaccine effectiveness” (28%), “No recommendation from health care providers” (27.5%), and “Too expensive” (21.3%) (Table 5). 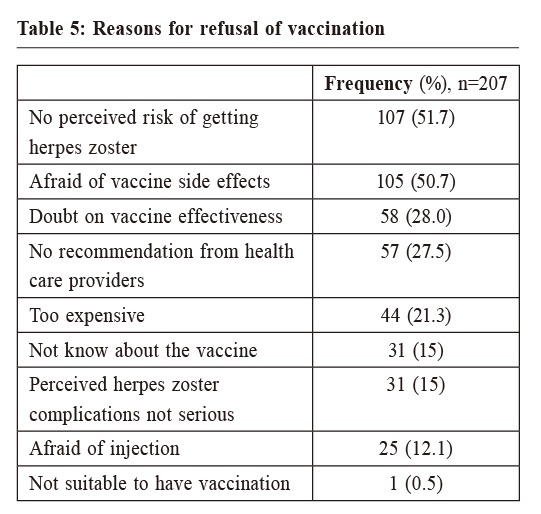 DiscussionIn the present study, we investigated the awareness of HZ, knowledge about HZ and its vaccine, and the HZ vaccination acceptance and the reason for and against injection among 400 participants attending a general outpatient clinic in Wan Chai district. We also analysed the factors which predicted HZ vaccination. Among our sample, 24.5% of all respondents had a history of HZ. This rate is higher than a local telephone survey (16.8%).18This prevalence is similar to a study conducted in Korea4. Although there was evidence that HZ vaccination is effective in reducing the incidence of HZ and PHN, only 12 out of the 381 participants had been previously vaccinated. The overall acceptance rate towards HZ vaccination in this study was 45.7%. It is slightly lower than the influenza vaccination acceptance rate (49.3%) conducted in a local study.11 Among the respondents who claimed they were aware of HZ, knowledge on HZ was just average, with only 72.4% answering 3 or more questions out of 6 correctly. In the unadjusted analysis, the group with higher knowledge scores had a 1.92-times higher vaccination acceptance (p=0.006) (95%CI, 1.20-3.05). Although the association became less significant in the adjusted analysis (p=0.059), it seems that efforts should be made on education about HZ and its vaccination if we hope to increase the vaccine uptake. We found that the HZ vaccine acceptance rate was 2.5 times higher in patients with a history of influenza vaccination the past 2 years (95% CI, 1.55-4.05). This positive association was also shown by other studies.2,3,14 One possible explanation is that this group of patient are more proactive in preventive care.14 Having a history of HZ was also a positive factor associated with the acceptance of HZ vaccination. The acceptance rate was 1.76 times higher (95% CI, 1.05-2.97). It seems that the fear or experience of HZ complications may have increased the demand for vaccination among these patients. The most common reason given in our study for not having the HZ vaccination was that there was no perceived risk of getting HZ (51.7%). The surveyed patients also reported concern on the side effects of the vaccine (50.7%). Other reasons for refusal of vaccination included “Doubt on vaccine effectiveness” (28%). These reasons were also reflected in research in other developed countries. 2,5 It seemed that our participants had misconceptions about HZ and the effectiveness of the vaccine, which was reflected in the knowledge test results. There were several limitations to this study. Firstly, data was collected by self-report, thus the past history of herpes zoster or history of vaccination could not be verified and might be at risk of recall bias. Secondly, we selected patients who visited the GOPC in Wan Chai, so most of the participants in this study lived in urban areas. Larger studies are needed in future to recruit participants in different districts for a more accurate estimation of prevalence, vaccination rates and attitudes to the vaccine to enable better generalisability. Thirdly, the design of this survey was based on a literature review but further testing is needed to ensure the validity and reliability of the results.  ConclusionTo date, there has been only a few studies conducted in HK to investigate the attitudes of patients towards HZ vaccine. Knowing the reasons for or against vaccination can help inform the government or health care providers on what information is needed to educate the public about HZ and promote uptake of the vaccine. From our study findings, it appears that greater public health education on safety and efficacy of the HZ vaccination is still needed and that there are common misconceptions that need to be addressed and corrected. Recommendation by health care providers appears to be an important influencing factor to enhance vaccination rates. Health care providers should seize the opportunity to promote HZ vaccination when patients attend for their influenza vaccination. AcknowledgementNo sources of funding were used to assist in the work of this research. Author disclosed no conflict of interest. The author gratefully acknowledged Dr Wong Man Ying, Michelle, Dr Tsui Pun Nang and Dr Leung Pui Sha, Crystal from the Department of Family Medicine and Public Health Care, Hong Kong East Cluster for their advice and support.
Long-yee Cheng,MBBS (HKU), FRACGP, FHKCFP, Diploma of Child Health (Sydney)
Correspondence to:Dr Long-yee Cheng, Fanling Family Medicine Centre, 1/F,
References:
|
|