|
December 2016, Volume 38, No. 4
|
Original Article
|
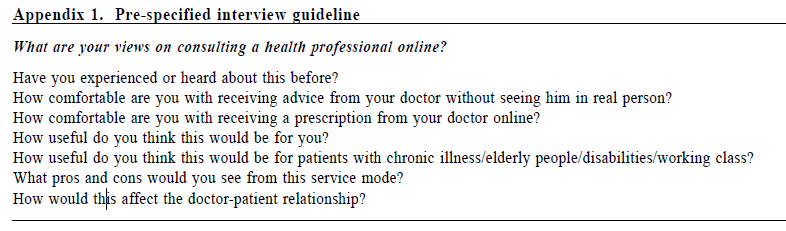
An exploratory qualitative study of patients’ views on medical e-consultation in a public primary care settingKenny Kung 龔敬樂,Hoi-fung Wong 黃凱烽,Julie Chen 陳芸 HK Pract 2016;38:120-127Summary Objective: Telemedicine is being effectively used to expand healthcare access to underserved populations and is also bringing added value to existing healthcare services. In Hong Kong, the use of telemedicine has been very limited. However, in those settings, it has been cost-effective and well-accepted by patients and healthcare professionals. In primary care, the selective use of e-consultation, as a form of telemedicine, may help enhance the healthcare accessibility of aging population with multi-morbidity and restricted mobility. This study aims to explore public primary care patients’ views on e-consultation in order to identify patientcentred issues which need to be addressed in planning such an initiative. Design: Face-to-face semi-structured interviews were conducted in Chinese or English. The interviews were audio-recorded and transcribed and the content was analysed for recurrent themes. Subject: 30 purposively selected primary care patients in a single General Outpatient Clinic (GOPC) in Hong Kong. Main outcome measures: Emerging themes from the interviews with participants. Results: Three key themes were identified: 1) advantages of e-consul tat ion; 2) concerns about e-consultation and 3) suggestions to improve the acceptability for e-consultation. Conclusion: Primary care pat ients have minimal experience with e-consultation, but are willing to accept its use to improve accessibility to healthcare if their concerns towards safety, security and communication are addressed. Further steps to explore the feasibility of e-consultation in primary care are warranted. Keywords: telemedicine, e-consultation, primary care, Hong Kong 摘要 目的:醫療機構可以通過遠程醫療在服務不足的地區有效 地擴展服務,同時令自身醫療服務增值。香港遠程醫療目前使用非常有限,然而它合乎成本效益並為廣大病人和醫護人員所接受。基層醫療中,選擇性地採用電子診療可幫助體弱多病和行動不便的長者使用醫療服務。本文探討公共基層病人對電子診療的看法,從而確定以後以病人為本原則制定先導計劃時需要處理的問題。 設計:以中文或英文進行半組織性的面談。會面過程錄音,再轉化成文字,根據重複主題做內容分析。 研究對象:香港一所普通科門診中30位經過挑選的基層病人。 主要測量內容:面談時參與者所提出的主題。 結果:三個主題確定為:(1)電子診療的優點;(2)對電子診療的關注;(3)改善電子診療認受性的建議。 結論:基層病人對電子診療的經驗很少,但是如果電子診療的安全性、保密性和通訊得以完善,他們還是願意接受 這種改善醫療服務的方式。電子診療用於基層醫療的可行 性可繼續探討。 關鍵詞:遠程醫療、電子診療、基層醫療、香港。 lntroduction Telemedicine (TM) or telehealth, the use of telecommunication technologies to provide medical information and services1, has expanded in many countries over the last decade, growing in both popularity and prevalence within the healthcare industry.2 While there was conflicting evidence about the effectiveness of TM in a 2010 systematic review3, individual studies looking at TM for specific disease entities have been more promising. TM was comparable with face-to-face consultations in the evaluation of primary care patients with low back pain4, promoted higher quality spirometry assessments5, resulted in greater reductions in depression severity6 and improved glycaemic control among diabetic patients.7 The research literature also suggested that TM helped to balance the healthcare workforce8 and to address manpower insufficiency.9, 10 A research team in the Netherlands explored TM in a shared care effort between primary care and specialist palliative care team clinicians.11 Patients and their caregivers had weekly videoconferencing interaction with the specialist and primary care physicians whenever possible. The results identified three key benefits offered by e-consultation, a specific aspect of telemedicine, which were 1) stronger encounter between the patients and their professional health care providers because patients are more willing to pour their hearts out with the distance created by the e-consultation, 2) improved insight into the patients’ daily lives for palliative care specialists, and 3) an intimate, trustful relationship from a long-term interaction.11 TM, as e-consultation, within Hong Kong’s public health services has been limited only to elderly home residents in certain districts12,13, where consultations via videoconferencing were used to replace conventional geriatric outreach or clinic-based services. A 200-bed geriatric nursing home has shown to be cost effective in reducing overall healthcare costs, improved access, reduced number of emergency department visits and reducing hospital bed-days.12 Moreover, these services were well accepted by both healthcare professionals and clients. The potential for the use of TM in primary care in Hong Kong, in particular e-consultation, has not yet been investigated. In this study, e-consultation is defined as patient consulting doctors through the use of telecommunication technology such as videoconferencing. For the aging population, who are suffering from multiple chronic diseases requiring regular public general outpatient services, and with increasing difficulty in going to the clinics due to their impaired mobility, illness, weather conditions or other logistical issues, e-consultation may be a means to supplement the care available in the current system. This study aims to explore primary care patients’ perspectives towards e-consultation, with a view to providing initial data to help inform the development of such an initiative. Method Study design and subject recruitment This was a qualitative study based on individual, face-to-face structured interviews with primary care patients. The interviews were conducted in January 2016. Patients were recruited from a local public primary care clinic with 250 patient-encounters per day. To assure a diverse range of views, patients were recruited through purposive stratified sampling of young, middle aged and elderly adults, (18-39, 40-65 and > 65 years old), representing participants in different stages of life, with a target of 10 subjects in each age group. Subjects had to be fluent in speaking Cantonese, Mandarin or English. One researcher (WHF) invited these selected patients to give informed consent to take part in the study. Recruitment of patients continued until the sampling quota was met and there was saturation of themes. Interview procedures The questions for the structured interview (Appendix A) were designed to explore participants’ views and experience towards e-consultation and were developed by family medicine specialists within the department based on the literature and points of relevance for the local setting. These guiding questions were first field tested in potential participants to ensure that items could be understood and interpreted correctly. The interviews were conducted by one researcher (WHF) with experience in qualitative analysis, and who was not involved in the clinical care of the patients. Each interview lasted 15-20 minutes, and all interviews were conducted privately in a consultation room of the clinic. The interviews were audio recorded with an MP3 recorder and transcribed verbatim. Data coding, and analysis of qualitative data Data were managed using NVivo 10 software (QSR International, Melbourne, Australia). We conducted a thematic analysis, aiming to identify a set of main themes that captured participants’ views. The approach to thematic analysis followed the framework outlined by Braun and Clarke.14 After the first few interviews, the authors began the analysis by independently documenting and then discussing the most salient observations from the interviews, which formed the basis of the initial coding framework. Two authors (KK and WHF) independently reviewed all transcripts and developed codes during the process. Using constant comparison15, similarity and differences in our data were highlighted, allowing for the establishment of analytical categories and key overarching concepts. Ethics approval The Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster approved the study protocol (IRB reference number UW 15-510). The study was conducted in compliance with the declaration of Helsinki. All subjects provided written consent upon participation. Results The recruitment process lasted for a month. Thirty patients were recruited to participate, of whom 12 were female and 18 were male. Their background characteristics are recorded in Table 1. The average interview time was 19 minutes (range 8 – 48). All interviews were done in Cantonese. There were 10 participants in each of the three proposed age groups. The average age of the participants in each age group was 26, 57 and 74 years old respectively. Saturation of themes was reached at this stage. Whereas the modal age is 24 in the youngest age group, 62 and 63 in the middle age group, and 67 and 69 in the elderly group. Their education level varies from no education to master degree holder. The youngest age group has the highest level of education, and the elderly group has little or no education, this is consistent with the demographic profile of the general population. Not many study participants were familiar with the idea of e-consultation and even fewer had experience in using it. Despite this, a large proportion of them still showed acceptance towards it and were able to give their views once the concept was explained. The three main themes identified from the content analysis, namely, 1) advantages, 2) concerns and 3) suggestions for e-consultations, are described as follows: 1) Advantages of using e-consultation (a) Convenience The most notable advantage of e-consultation expressed by participants is convenience, with participants believing that there will be shorter waiting times for consultation. Receiving a diagnosis at home would save more time, as one participant mentioned: “It [e-consultation] is more convenient and I don’t have to waste my time coming in for check-ups … if you don’t have any serious problems, the doctor usually speaks to you briefly then you can go.” [Civil Servant, male, age 40 – 65] “I think seeing [a doctor] on the internet is fine, given that my disease is not severe. I think this is very convenient” [Civil servant, retired, female, age 40 – 65] One participant felt e-consultation could break down the geographic barriers that potentially reduce access to health care: 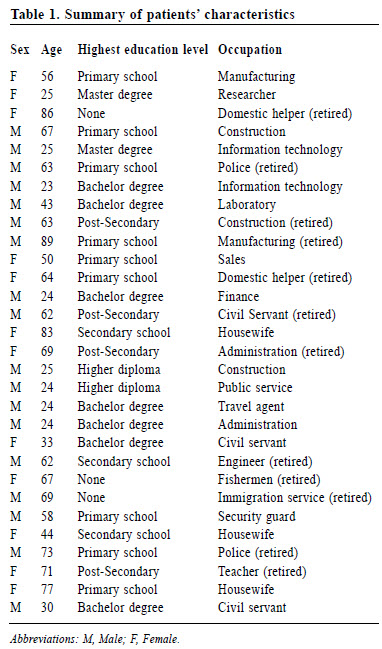
“Sometimes a particular specialist is in another city, then he can save people’s life by consulting the patient or tutor other doctors on the internet.” [Administration, retired, female, age above 65] E-consultation is considered by some participants to be convenient especially for certain subgroups of patients: “I think it [e-consultation] is more convenient. Especially to elders who have difficulties in walking, travelling to the clinics for a regular check-up is very time-consuming.” [Finance, male, age 18-39] (b) Better communication Some participants felt it would be easier to speak to a doctor via a computer. They believed they could have a longer consultation, allowing them to ask questions which they would not have time to ask in a traditional consultation: “I think e-consultation will not be limited by the time, so it will be a family doctor that is closer to you.” [Construction, male, age 18-39], One participant pointed out that e-consultation would be helpful for discussing sensitive problems with the doctor: “When I need a gynaecologist, due to the one I have near home is a male doctor, I would rather do it online.” [Civil Servant, female, age 18-39] (c) Healthcare system efficiency Some described how e-consultation could benefit the healthcare system. They believed the service could reduce the number of patients in the hospital by treating them online: “I think it [e-consultation] is good, good for the patients and doctors. And the hospitals won’t be crowded. If everyone goes to a hospital for all sorts of problems, then they are misusing the system. They are affecting those who are actually in need...” [Manufacturing, retired, male, age above 65] Most patients agreed with using e-consultation as a tool for triaging as one participant described: “I think it [e-consultation] is useful, by separating patients by severity. Most patients in the outpatient clinic are just simple cold, and some are chronic disease patient that only require long-term monitoring.” [Construction, retired, male, age 40-65] “It [e-consultation] is good. The hospital won’t be as crowded as it is now. Those who need medical attention can benefit from this.” [Civil Servant, female, age 18-39] 2) Concerns about e-consultation that prevents patients from choosing e-consultation (a) Technical and logistical issue Those who questioned the reliability and feasibility of e-consultation raised a few concerns or issues that would prevent them from using the service when e-consultation was mentioned to them. Some did not know how to access the internet or did not have a computer as two participants stated: “[After learning what e-consultation is] I don't know how to use the internet.” [Housewife, female, age above 65] “[After learning what e-consultation is and what it requires] I can't read and don't have a computer.” [Domestic helper, retired, female, age above 65] (b) Lack of personal interaction Some participants preferred the traditional way of consultation with the direct face-to-face contact with the doctor when they were asked how comfortable they were with e-consultation: “I have heard of it before but it doesn’t sound real to me. It could be a trend in the future but I don’t think it is better......I don’t feel this can work and doesn’t feel real to me. I prefer going to a doctor in a clinic, let the doctor see myself through his own eyes.” [Manufacturing, Female, age 40-65] Most who doubted the usefulness of e-consultation were concerned with doctors’ inability to provide handson physical examination during the consultation, which the participants saw as a disadvantage: “E-consultation can only see the outer you. They cannot see the inner problem, for example, you told him [the doctor] this part of your body is hard and you felt pain, he still wouldn’t know what it is, unlike face-to-face seeing him then he can touch you and find out what it is. Without actually touching you he cannot provide you with a definite answer on what disease you might have.” [Immigration agency, male, age above 65] Participants doubted their reliability in the selfreporting of their symptoms, believing that Chinese in general are less competent than other populations in verbalising their problems properly, described by one participant: “I think it [limitation in e-consultation] is to do with our culture, the whole Asian population isn't that verbalised. Sometimes a doctor needs to dig information out from the patient, yet they may not be able to express accurately. Therefore, I don’t think this can solve the patient’s personal problem [without seeing the patient] because not all symptoms are apparent.” [Research, female, age 18-39] Poor communication is likely a cause of mismatch in the communication, leading to incorrect diagnosis. A participant pointed out that symptoms shared by multiple diseases also added difficulties in making an accurate diagnosis: “I think it [e-consultation] can be difficult to distinguish some disease that has the same symptoms.” [Information technology, male, age 18-39] (c) Concern with cyber security and safety When asked about how comfortable they would be with advice from e-consultation, some participants described the service as unrealistic, unsafe and unreliable. Collectively, they showed a lack of trust in the diagnosis delivered by the service: “[When e-consultation is mentioned] the internet is very unrealistic. The things they said on the internet are very unreliable. I prefer they give me the address of the doctor so I can go there directly.” [Police, retired, male, age above 65] A few participants had concerns with the internet security, which could have an impact on privacy: “If you forgot to take safety measures then you will expose your privacy to risk.” [Police, retired, male, age above 65] These participants raised a question on how to ensure the doctor making the diagnosis could be authenticated, with this quote extracted from a participant: “ One concern is that it [the person on e-consultation] might be fake. I think this is the grey area of this service.” [Manufacturing, female, age 40-65] One participant believed this would be a flaw that could be exploited by criminals, damaging their trust towards the service: “I think e-consultation opens up an opportunity for criminal activities if safety measures [online security] are not taken.” [Police, retired, male, age above 65] (d) Issues with prescriptions Concerns about getting a prescription after e-consultation were asked by our participants: “I think the only problem is you cannot get the medication immediately…” [Civil servant, female, age 18-39] Collaboration with community pharmacies is a possible means of facilitating timely prescriptions; however, some participants were distrustful of the local pharmacy, describing them as unprofessional: “The problem [for receiving online prescription] is where we buy the drugs. Most of the pharmacy store outside sell fake products.” [Construction, retired, male, age 40-65] Even with the public government dispensary, participants were worried by the possibility of mistakes in dispensing: “I am concerned with the risk of receiving the wrong medication.” [Public service, male, age 18-39] 3) Suggestions to improve acceptability of e-consultation (a) More user support Although some participants were against e-consultation because of difficulty with internet access, they would consider using the service with the help from family members and friends, as this participant described: “It [e-consultation] is only feasible if I can receive help from the younger ones, helping me to use the internet…” [Fishermen, retired, female, age above 65] They even expressed the willingness to learn using the service if it was simple enough: “[Discussing the use of e-consultation] People like me who live by myself won’t get any help. I have to rely on myself, but I would still use it [e-consultation] as long as it is not too difficult to learn.” [Manufacturing, retired, male, age above 65] (b) Selective use While the inability to provide hands-on physical examination was of concern, participants pointed out that this would not be an issue if their condition was mild or if the consultation only involved a simple follow up. “I think you can make your own judgement on choosing which service depending on the severity of your illnesses. For patients with chronic illnesses who have to visit the clinics regularly, e-consultation may be more suitable for them.” [Finance, male, age 18-39] At the other extreme, some participants felt that if their health condition was so poor that they had difficulties leaving their homes, e-consultation would provide ready access to healthcare: “Well maybe if I am so ill and find it difficult to walk out of my bed, then I can give it [e-consultation] a try...” [Information technology, male, age 18-39] Furthermore, adequate doctor-patient communication and the availability of comprehensive patient medical records are seen as ways to reduce this lack of physical touch and enhancing diagnostic quality: “ Although the doctor can only ask without touching, but this is not a problem if you can deliver the message clearly.” [Administration, retired, female, age above 65] “On the internet you have to tell the doctor your symptoms… with a detailed medical record would give me greater confidence.” [Police, retired, male, age 40-65] (c) Government regulations Governmental regulations in the establishment and running of e-consultation services would enhance participants’ trust in the service. “As long as the government is at the back of the service [e-consultation], I would then have confidence in it.” [Domestic helper, retired, female, age 40-65] These include the clamping down on any illegal activities, ensuring doctor credibility, and monitoring private pharmacy services: “If the website is under the Hospital Authority or other official bodies which has some security measures, then the reliability will be higher.” [Housewife, female, age 40-65] “There are so many frauds in these private pharmacies, therefore the government needs to have more regulations on them.” [Civil servant, male, age 18-39] (d) Practical issues Although effectiveness and quality were regarded as essential features for the use of e-consultation by participants, this would require time to establish: “It depends on if it [e-consultation] works or proved as worked, but I would not be a Guinea pig.” [Information technology, male, age 18-39] “Depending on the treatment effectiveness, I will gain or lose confidence in the service.” [Construction, retired, male, age 40-65] Cost was a concern as mentioned by this participant: “As long as it is cheaper than the private clinics… and I think the price should be standardised if you are doing e-consultation. Do not imply extra charge.” [Civil servant, female, age 18-39] Some participants demanded high internet stability for the service, as they felt it would be useless if the technology itself was unreliable: “ If the computer system is slow then it [e-consultation] isn’t helpful. It will take longer if the computer system constantly breaks down and need to spend hours to recover.” [Laboratory, male, age 40-65] Being able to obtain a sick leave was also a factor that patients thought was important when considering e-consultation: “Someone needed a sick leave would prefer the traditional way of consultation because he needed the doctor's signed an approval letter. What if the doctor does not give him the letter after saying his condition is mild [with e-consultation]. This needs to be considered.” [Civil servant, male, age 18-39] Discussion To our knowledge, this is the first study in our locality looking into e-consultation in primary care, focusing on collecting patients’ perspective on the advantages and potential barriers for developing this service in Hong Kong. Experience with e-consultation was minimal among our sample of public primary care patients, a finding that is consistent with the lack of provision of related services in Hong Kong. Nevertheless, our structured interviews have provided us with insight towards the needs of potential service users. The advantages identified by our interviewees are compatible with existing literature, particularly in relation to increased accessibility to specialist advice, less traveling required, and reduced waiting time.16 Patients felt communication with doctors would be easier through e-consultation also reinforce the previous findings by the research team in Netherland, but our patients did not feel the intimacy with doctors will change11, which could be explained by the cultural differences between the two groups of patients. From our results, it seems that the implementation of e-consultation requires authorities to address issues concerning data security, safety, doctor-patient communication and remote physical examination. Our participants’ concerns towards data security and safety were mostly related to credibility and data privacy. As a matter of fact, security encompasses a multitude of problems including authorisation, authentication, accounting17 as well as data privacy and physical safety.18 E-consultation has been considered to differ from the classical medical consultation in reducing personal contact and running the risk of alienating the patient21 with resulting increase in dissatisfaction. Since the increase in utilisation, systematic reviews have shown that patients reported high levels of satisfaction towards e-consultation.16 Physical examination during e-consultation is feasible with current technology, with literature suggesting that there is minimal difference between examinations performed during face-toface consultations and e-consultations. Comparison of conventional consultation and telemedicine consultation for managing heart failure indicate findings are identical or similar20, although reliability decreases under the hands of clinicians inexperienced with e-consultation.21 Current literature suggests that e-consultation is clinically effective and results in a better control of blood glucose in diabetics when compared with face-toface or telephone delivery of care.20 This evidence helps to dispel our participants’ concerns about impaired doctor-patient communication and effectiveness of e-consultation. Nevertheless, cultural and individual differences will exist and authorities and clinicians practicing e-consultation in the future must take these concerns into consideration during the implementation of these services. Our participants identified the importance of adequate computer and online access in conjunction with appropriate skills training in improving e-consultation’s acceptability. This is of particular concern among the elderly since many of them in our locality do not have computers at home.22 Despite their lack of computer knowledge, elderly patients are known to be receptive to new technology particularly in terms of electronic health.23 Given our elderly patients’ willingness to take on new knowledge, ensuring hardware accessibility and user-friendly software or applications are essential. The strengths of this study include the fact that it is the first study of this kind on e-consultation in Hong Kong, where telemedicine is still in its infancy. There are limitations in our study. Although we have attempted to increase generalisability through purposeful sampling, our patient recruitment was limited to only one primary care clinic. While further studies should include participants from other regions of Hong Kong, the views obtained from our participants should have already given healthcare providers with important insights into the future development of e-consultation. Apart from patients, the opinions from healthcare professionals should be obtained in future studies. 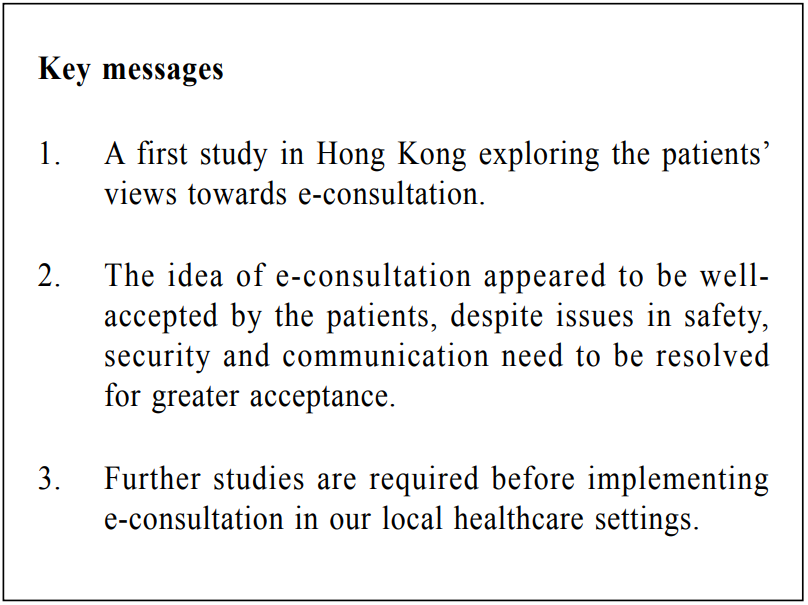
With the development of electronic health record and telehealth service in geriatric outreach in Hong Kong, further expanding e-consultation service to primary care may enhance patient care and boost the efficiency of the health care system. Conclusion Despite having minimal experience with e-consultation, our primary care population appears to accept its use to improve accessibility if their concerns towards safety, security and communication are addressed. Further steps to explore the feasibility of e-consultation in primary care are warranted given the untapped potential benefit which technology can bring to health care.
Kenny Kung, FHKAM, MRCGP, FRACGP
Clinical Assistant Professor Department of Family Medicine and Primary Care, the University of Hong Kong Hoi-fung Wong, MPH, BSc (Hons) Research Assistant Department of Family Medicine and Primary Care, the University of Hong Kong Julie Chen, FCFPC, C.C.F.P., M.D. Assistant Professor Department of Family Medicine and Primary Care, the University of Hong Kong Correspondence to: Dr Julie Chen, 3/F., 161 Main Street, Ap Lei Chau Clinic, Ap Lei Chau, Hong Kong SAR, China. E-mail: juliechen@hku.hk
References
|
|