December 2012, Volume 34, No. 4 |
Update Article
|
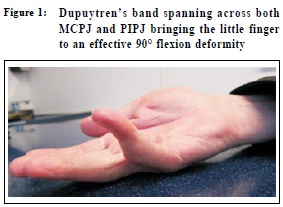
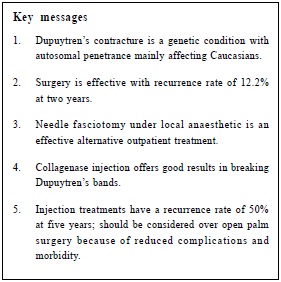
Dupuytren’s contracture: management updateDaniel WH Mok 莫華康 HK Pract 2012;34:145-149 Summary Dupuytren’s contracture is uncommon in Asians but still presents in sufficient numbers to primary care doctors. The time honoured technique of open palm surgery is now being challenged by newer injection techniques which can be performed in outpatient clinics under local anaesthetics. The article discusses recent advances made in the understanding of the etiology and updates treatment of this benign and yet progressive condition which can cripple the hand. 摘要 筋膜攣縮在亞洲人中並不常見,但是基層醫生仍然有機會接觸此類病患。曾風行一時的開掌手術,現在受到了 挑戰,病人可以在局部麻醉下在門診進行注射治療。本文討論了此病的病因以及治療的最新進展,本病雖屬良性,但有進行性的發展趨勢,可造成手部殘廢。 Introduction Dupuytren’s contracture is a form of fibromatosis of unknown etiology. Excessive fibrous bands and nodules develop within altered connective tissues of the palm and fingers. The majority of patients only suffer a mild form of the condition. Some resultant contractures invariably interfere with daily function (Figure 1). It was first described by French surgeon Baron von Dupuytren in Paris in 1832. The condition is common in Northern Europe, North America and Australia, and is reported in the US and Germany to occur in about 3% of the working population;1 its incidence rises with advancing age. After the age of 50, the condition affects 17% of men and 18% of the patients are female. Genetic factor plays a part as 40% of patients have a family history. Environmental factors such as injuries, as well as diabetes, epilepsy, alcohol excess, smoking, HIV infection and hyperlipidemia may play a part intriggering onset of this condition.2 Etiology The concentration of hypoxanthine is found tobe six times higher in the palmar fascia of patients with Dupuytren’s contractures than controls.3 Xanthine oxidase, which is located in endothelial cells of the microvascular network, is released in response to trauma and local ischaemic condition, and reacts with hypoxanthine to form superoxide free radicals (O2-). The free radicals stimulate fibroblasts proliferation with forma t ion of Type III collagen instead of Type I. In addition, they stimulate cytokines such as Interlukin-1 (IL-1), which acts on Transforming Growth Factor-β (TGF-β) in the Dupuytren’s tissues, bringing about myofibroblast proliferation and fibroblast differentiation. The result is rapid development and contraction of Dupuytren’s bands. Pathoanatomy The disease most commonly affects the ring finger, then the little finger. Bands can also develop in the firstweb space between the thumb and index metacarpalheads. Cords tend to run from the flexor retinaculumtowards the middle of the middle phalanx. Recent advances Radiotherapy Radiation therapy to early Dupuytren’s nodules and cords may delay the growth rate of the fibroblasts within the palm. The dose is normally 15Gy over 5 days. This contrasts with normal radiation dose of 30Gy or more for tumours treatment. The effect of radiation is uncertain and unpredictable. In a randomized control trial, 129 patients with 198 hands were treated with either 30Gy or 21Gy. Review at 1 year showed objective improvement in 56% and 53% respectively. Regression of disease was noted by 85% and 53%. Patients should be made aware that there is a theoretical long term risk of malignancy after any type of radiation therapy. Radiation dermatitis, such as dry skin, desquamation as well as altered pain and temperature sensation were reported at 3 months’ follow-up in 16% and 11% respectively.4 In another series of 135 patients with 208 hands treated with radiotherapy, 59% reported that their conditions were stable and 31% noted their disease progressed at 13 years. Mild skin atrophy with telangiectasia were reported in 7% and minor skin dryness and increased desquamation in 23% at 13 years. Palmar fasciectomy and needle fasciotomy are required when radiation fails. Radiotherapy may be beneficial in reducing recurrence after needle fasciotomy. Steroid Injection Ketchum et al investigated the results of steroid injection into palmer Dupuytren’s nodules.5 After an average of 3.2 injections, nodules softening and flattening were noted in 97%. Sixty to 80% experienced definite but incomplete resolution of the nodules, while 50% experienced reactivation of disease in the nodules 1 to 3 years after the last injection, necessitating 1 or more injections. The findings of this study indicate that intralesional injection of Dupuytren’s nodules with triamcinolone acetonide may modify disease progression. Allopurinol and Colchicine Allopurinol binds to xanthine oxidase, preventing the release of free radicals and stops the proliferation of fibroblasts and myofibroblasts. Progression of Dupuytren’s contractures is then halted. Colchicine has been shown to stop collagen synthesis from the fibroblasts and at the same time stimulate collagenase production. A pilot study involving 10 patients concluded that colchicine treatment was effective in the treatment of Dupuytren’s contracture.6 Surgery Non-painful nodules do not require excision. Patient’s inability to place his hand flat on the table is often an indication for intervention. This usually means there is more than 30° of contracture at the metacarpal phalangeal joint (MCPJ) or any degree of flexion contracture at the proximal inter-phalangeal joint (PIPJ). In palmar fasciectomy, the diseased fascia and cords are excised. This necessitates multiple skin incisions over the palm under general anaesthesia. Prolonged hand splinting, with many weeks off work and driving are to be expected after surgery. In cases where all the Dupuytren’s tissues cannot be removed or if wound closure was not possible, the use of local or distant skin grafts may become necessary. In dermato-fasciectomy, the overlying skin together with the underlying diseased fascia is resected, in the belief that the dermis is also involved. Full thickness skin graft is used to cover the defect and is generally reserved for severe PIPJ contracture. The recurrence rate for fasciectomy and dermato-fasciectomy at three years reported by Ullah et al were the same at 12.2%.7 Additional full thickness skin grafts did not offer better correction or reduce recurrence. It is now reserved for the management of recurrent disease.
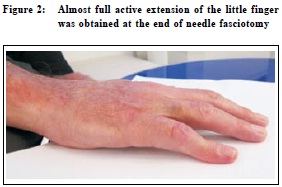
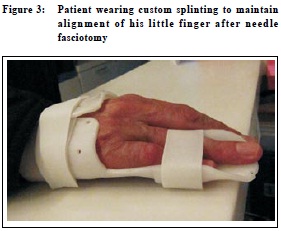
This is a minimally invasive technique pioneered by French rheumatologist Lermusiaux thirty years ago.9 Because of the high recurrence rate after open surgery, a simple office procedure under local anaesthetic received renewed interest. He used a needle to break and transect the cords in a side to side manner at different levels in the finger and the palm. Passive stretching and manipulation ensure breakage of the bands. The procedure takes twenty minutes, and the patient can return to drive and work the following day. Recreational sports, such as golf, can resume after three days. Complications are uncommon. Digital nerve injuries, skin lacerations and delayed tendon rupture are rare and have been reported to occur at less than 1%. Van Rijssen et al have reported 85% recurrence at five years at a mean of 2.3 years.10,11 The high recurrence rate is expected, as this technique does not remove any diseased tissues. Collagenase Clostridium histolyticum (Xiapex-Pfizer Limited) Collagen bands can be dissolved when injected with this bacterial enzyme. In a prospective study involving 300 patients, cords were injected with collagenase and manipulated up to three times at monthly intervals.12 77% correction was obtained in the MCPJ and 40% in the PIPJ with collagenase, contrasting with 7.2% and 5.9% in the placebo group. Complications include pain secondary to the injections and manipulations, local swelling, bleeding, skin lacerations and regional lymphadenopathy. Tendon ruptures have been reported. Nearly all patients developed anticollagenase antibodies. The only reported immune reaction is pruritis, reported by 11% of the patients in the trials.13 The long term autoimmune response to repeated injections and recurrence rate are unknown. For now, it appears to be a simple and effective means to treat Dupuytren’s cords, particularly those across the MCPJ. Nevertheless, the drug is not available for general release in Asia. Hand therapy and Splinting Dupuytren prescribed night splints for his patients after surgery and observed excellent results. Since then, postoperative splinting has been an accepted protocol. For needle fasciotomy, Albrecht Meinal reported correction of the most resistant cords after fasciotomy followed by six months of night splinting. He lined his splints with silicone and remoulded over time to gain correction.14 Over extension should not be attempted as the micro-circulation can be compromised which in turn lead to the release of free radicals. The hand should be given an opportunity to have daily flexion exercise. The wound should be massaged with putty to reduce oedema and discourage excessive scar tissue formation. Splinting forms an important part of treatment to control recurrence after needle fasciotomy. Recurrence As none of the above treatment is curative, recurrence of Dupuytren’s contracture is inevitable. In a retrospective study of 216 patients treated after a minimum of two years, Degreef reported 54% recurrence in all surgical procedures.15 43% were seen in palmar fasciectomy and 63% in dermato-fasciectomy. Recurrence is associated with many risk factors, including patients under the age of 50, bilateral disease, positive family history, and the first ray as well as subsequent multiple rays involvement, and nodules at ectopic sites, e.g. Ledderhose, La Peyronie’s disease.16 Costs In 2011 , with calculations based on an expected-value decision analysis model, Michigan Medical School concluded open partial fasciectomy is not a cost-effective treatment when compared with needle fasciotomy and collagenase injections.17 At the time, each vial of collagenase for injection was priced at HK$7,320, the doctor’s fees not yet included. The cost of this treatment was therefore more expensive when compared with needle fasciotomy but still a fraction of that of open fasciectomy which also necessitates a visit to the operating theatre and the service of an anaesthetist. Author’s experience Technique of needle fasciotomy The “tensioned” areas of the bands are palpated and labelled with a skin marker. The hand is then cleaned with 10% Povidone Iodine (Betadine) solution. 1% Lignocaine is used as local anaesthetics to infiltrate the bands at the marked areas. Using 0.5x25mm 25 G needle, the bands are transected with the needle in a side to side manner, taking precaution not to damage the flexor tendons which are at a slightly deeper level. Over the proximal phalanx, attention should be paid to the digital nerves which cross over the Dupuytren’s bands at this level. Referred pain down the digit will be felt if the nerve is accidentally touched upon. In a consecutive series of 23 patients with 38 digits affected by Dupuytren’s contracture treated with needle fasciotomy in 2007-8, followed up at six months showed a 90% successful correction in 30 digits with primary disease, and 62.5% good outcomes in 8 digits which had previous open surgery. Complications included pain during injection in two patients, skin lacerations in two and parathesia in one. Flexor tendon injuries were not present in this series. No recurrence was seen at 6 months. Patients interviewed were all satisfied with the treatment; except one who needed to undergo the same procedure again. Recommendation The benefit of needle fasciotomy is that it is a short outpatient procedure without the need for general anaesthesia. It has a low complication rate (less than 1%) with minimal scar tissues formation. In cases of recurrence, the procedure can be repeated. Return to normal daily activities is almost immediate. The procedure should be performed by an experienced doctor. Despite a high recurrence rate , needle fasciotomy remains a recommended procedure by the National Institute of Clinical Excellence in the UK.18 Daniel WH Mok, MBBS (Lond), FRCS (Ed), FHKAM (Orth) Correspondence to: Dr Daniel WH Mok, Room 2906 Bank of America Tower, References
|
|