|
April 2007, Volume 29, No. 4
|
Original Articles
|
The cycle fear: a qualitative study of SARS and its impacts on kindergarten parents one year after the outbreakWilliam C W Wong 黃志威, King-chi Chan 陳敬志, Hiu-wai Tang 鄧曉煒, Michael W H Lam HK Pract 2007;29:146-155 Summary
Objective: The outbreak of severe acute respiratory syndrome (SARS)
in 2003 killed 299 people in Hong Kong and resulted in tremendous psychological,
social, and economic impacts. Design: Qualitative Study.
Keywords: SARS, stigmatization, behavioural change, Hong Kong. 摘要
目的: 在香港2003年的嚴重急性呼吸道綜合徵(SARS)爆發引致299人死亡,而且令民眾心理,社會及經濟受到嚴重打擊。
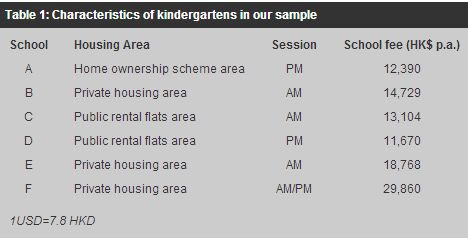
主要詞彙: 嚴重急性呼吸道綜合徵(SARS)、被標記、行為變化、香港。 Introduction The epidemic of severe acute respiratory syndrome (SARS) imposed tremendous social, psychological, and economic stress to the Hong Kong society.1-4 The restrictive infection control techniques such as quarantine and isolation employed to protect the public, although very effective, exacerbated the psychological burden of individuals.5 In particular, people were struck with a deep sense of dismay at the suspension of classes6 and the evacuation of all residents in block E of Amoy Gardens to quarantine camps following a large scale outbreak in that building. The panic level of the general public culminated after the World Health Organization (WHO) announced travel advisory warnings against Hong Kong and Guangdong Province on 2 April 2003.7 Majority of the public indicated they felt helpless, horrified and apprehensive.8 In response to the health crisis, some people implemented appropriate preventive practices,9 while many others adopted extreme preventive measures in response to the high level of anxiety.10 A number of medico-sociological models were applied to explain these behavioural changes, for example, the health belief model which was used to predict rational protection behaviour toward SARS.11 Another study showed the theory of planned behaviour explaining a portion of variance in nurses' intention and volunteering to care for SARS patients.12 However, the associated stigma (a critical factor in affecting health behaviour) which might have interacted with fear and social harmony was not addressed in those models. During the SARS epidemic, the Equal Opportunities Commission of Hong Kong received more than 520 inquiries and complaints from the public about possible discrimination related to SARS.13 With the avian flu pandemic impending globally,14 urgent and effective measures must therefore be established by the government and health professionals to mitigate the unnecessary fear and stigma arisen from infectious outbreaks. By focusing on the parents of kindergarten children, this study attempted to seek a link between stigma, fear, and other factors involved in the SARS epidemic. This group of people was selected because they faced particular difficulties during an infectious disease outbreak in that they had to take care of the young, vulnerable children who were unlikely to perceive the threat of the disease or to protect themselves adequately. Therefore, we explored the perception, associated behavioural change and the underlying rationale for such, sustained practices on disease prevention, and comments on the general epidemic control of the parents of kindergarten pupils one year after the SARS outbreak. This study was conducted at the time when the experience of SARS began to be valued and understood while the threat of another outbreak was real.15 It was anticipated that the findings would provide invaluable insights to Hong Kong and other countries when challenged with other novel infection outbreaks such as avian flu. Methods Purposive sampling of kindergartens in Shatin district of Hong Kong, one of the most severely affected areas by SARS, was adopted. A total of 61 registered kindergartens were found in the 'Profile of Kindergartens (Shatin) 2002-2003'.16 Stratification of the samples according to housing types in the geographical location, school sessions (am/pm), and school fees were performed to ensure fair representation of different social classes and background. Six out of eight randomly chosen from the stratified kindergartens (75%) accepted our invitation (Table 1). The two selected but refused kindergartens indicated that a tight scheduling problem prohibited their cooperation. Six to eight parents were invited to join a discussion on SARS in their respective schools.
A qualitative study by means of focus group interviews with parents was adopted. From 27 May to 22 July 2004, six focus group (40 females and 4 males) interviews were held in different kindergartens with the interview time ranging from 60 to 90 minutes (with a mean of 77 minutes). Verbal consent was obtained before each focus group discussion began, and the discussion facilitated by a semi-structured questionnaire that covered five main areas including the informants' attitude toward SARS and their rationale behind such feelings; how they acted to protect their children, themselves, and their other family members from the disease as well as access to and opinion of the health information about SARS and finally, how SARS had changed their attitude and behaviour in all aspects of life. Two researchers acted as facilitators in all the focus group discussions to avoid inter-group variability. An observer with an anthropology background was also present to make field notes and audiotaped the content of the discussions. The recordings were later transcribed for analysis. Themes and ideas generated from the interviews were analyzed using the Grounded Theory.17 The researchers started with broad headings, then identified more detailed codes before deciding on higher-order headings. Some of the themes were based on the descriptive codes which were derived directly from the responses to the interview questions, while the others were more interpretative based on the data from a number of questions. Themes (categories) and different properties (subcategories) were set out after the interview with the first focus group to allow emerging theories. The relationships between themes and properties were grouped and analyzed in order to identify the link between the themes and to devise a model to explain a social phenomenon in the outbreak of a new disease. The quotes were translated into English and then back-translated by an independent individual. The group number to which the quotes were arisen from was added at the end of each quote. This study was approved by The Survey and Behavioural Research Sub-committee of the Chinese University of Hong Kong. Results 1. Fear of uncertainties The core themes generated from the focus group discussions were centered on the deep sense of "fear". The origin of fear was derived from the general uncertainties of the disease: uncertainties regarding the disease's origin, its mode of transmission, treatment, prognosis and adverse effects of the treatment which had attracted a lot of public attention. "I heard there would be a lot of side effects (of the treatment) like osteoporosis, for instance. Bearing this in mind I was still young, I told myself that I would rather die." (Group 2) Stigmatization and fear was amplified when the general public perceived their medical professionals were in great fear and were losing control. This vicious cycle of fear perpetuated resulting in greater panic and perhaps even increased infection cases and social conflicts. "After he went to the doctor, he was more frightened. The doctor was probably overacting and exaggerating things. I only wore a mask, while he wore a full suit which showed only his eyes. If you were me, would you be frightened? It was really terrible." (Group 5) "Doctors were frightened, not us. The doctor said, "What problems do you have? You do not need to stay that close! Enough! Enough!"(Group 4) Another reason for fear was the guilt associated with infecting other people. Some informants indicated that they did not fear death, but they worried infecting others especially their family, children or even the general public. "I would not know it if I was infected. If I have infected 10 of you here, I would feel guilty. There is fear of isolation and the side effects after the treatment (of SARS) more than death itself. Actually, a lot of people are not afraid to die." (Group 2) 2. Emotional disturbance During the epidemic, people were under different degrees of emotional disturbance ranging from worry to stress, anxiety and panic. The psychological reactions to the epidemic had both short and long term effects, as well as some positive and negative behavioural changes in people to combat the disease. The majority of parents expressed worry about their young children and became more fearful when the death toll was increasing. Some long-term psychological damages were evident in the following statements: "Really anxious, I could burst into tears when I sat alone. It (SARS) made me feel trapped, and I did not know what would happen. It was not advisable to go out, or even to take the lift. It was miserable." (Group 6) "My younger son was born in February (2003). In the past, with my elder son, we often visited relatives and friends, but during the SARS outbreak and for at least a year, we did not take our baby out, so his 'personality' became different. He's scared of seeing new faces."(Group 6) 3. Rational behaviour changes and better self-control Some rational behavioural changes were noted among the public including improvement in general health awareness, personal hygiene (wearing a mask when sick, disinfecting the living area, washing hands properly and frequently, using communal chopsticks, avoiding crowded places, etc) and lifestyles (healthy diet and more exercise). It also contributed to enhancement of self-discipline. Some of these changes were still sustained one year after the SARS epidemic. "Now I would wear a mask when I am sick, and I wash my hands frequently." (Group 1) "Now I would do more exercise- health is the most important thing." (Group 1) "I believe the lesson (to have learned from SARS) is to have greater awareness of a crisis. It was really good that we had it, while we could still help ourselves." (Group 3) 4. Inappropriate changes in health seeking behaviour and stigmatization Nonetheless, many behaviours derived from fear were detrimental to the control of the epidemic and upset social cohesion. Avoidance (by keeping away from the perceived high-risk group) was a common strategy people adopted to respond to the epidemic. Some informants avoided seeing a doctor when they had symptoms resembling SARS. In less extreme cases, some even delayed their regular medical or dental appointments, and chose to self-medicate, or visit doctors far away from their home in a non-epidemic area. "She had a colleague who admitted two patients. They did not mention that they were living in Amoy Gardens and went to the North District Hospital... After admission, it was later discovered that they were living in Amoy Gardens. Then everyone was afraid of getting infected (with SARS)." (Group 5) Poor coordination existed between the pubic and the private health care systems. Private hospitals refused admissions of suspected cases and these discriminating actions generated more irrational health-seeking behaviours among the general public. They believed that the suspected SARS cases would either be sent to a hospital for isolation or that the likelihood of being infected with SARS in a clinic or hospital was high. Some medical professionals overreacted by exhibiting a discriminatory attitude towards their patients. "Her husband did not have SARS- it could have just been typical pneumonia. It happened in a private hospital called the Baptist Hospital in Kowloon Tong. When the official X-ray showed his chest was infected, he was refused admission. He was then self-isolated at home and dared not seek further medical treatment. He felt the Baptist Hospital had rejected him and assumed if he had SARS, he could only wait (to die) at home..." (Group 6) "Once you got admitted into a hospital, every doctor would treat you as a SARS patient: they'd give you injections everyday, and then you also had to wear an N95 mask 24-hours-a-day. I was terrified!" (Group 5) Normal social life such as going out for shopping, eating, working and/ or leisure activities were severely disturbed during SARS. Interpersonal relationships (even for close relatives and friends) were greatly affected. There was an impression that the "invisible" carriers of SARS were present everywhere and no one could be trusted. A woman whose husband is a doctor recounted her experience as, "Once he (her husband was a doctor) opened the door, he would go straight to the toilet, clean himself thoroughly, and hang his clothes outside the house for airing. He did not touch the kids, also did not quite touch me, and we ate separately." (Group 6) "The trust between people became so alienated that it had changed to reciprocal guessing." (Group 3) Some informants became so paranoid that they began to suspect everyone was a SARS patient, especially the elderly people who had been portrayed as "invisible" carriers by the media. Consequently, some severely sick people isolated themselves to avoid being stigmatized, and the stigma that hovered over society during the epidemic hindered the identification and treatment of patients. "The building he lived in had a (SARS) case, so he went to a hotel. When he was in the reception area, one of his family members coughed, and the hotel sent them away and said, 'Sorry, we do not serve patients'." (Group 6) "He had a fever and was getting more and more uncomfortable, after measuring his temperature, he said, 'I could not make it, I must self-isolate', then he locked himself up in his room." (Group 6) 5. Other irrational behaviours Irrational behaviours like overreactions, blaming, denial, and seeking irrational medication were noted during the epidemic. All these behaviours were responses to the fear, which became self-perpetuating at the same time. The situation had a massive impact on personal life and social harmony. Examples of these overreactions included people rushing to the supermarket to stock up on food; using disinfectants excessively and obsessively, and washing repetitively: "My child was very nervous. There was a sink in their classroom, his teacher was very nervous about him and made him wash his hands before class, after meals; he washed hands after art class; at most times he had to wash his hands; he used soap lotion, scrubbed for a long time." (Group 6) "Sometimes when inside the house, the child diluted a disinfectant solution and sprayed aimlessly into the air! He sprayed above the bed as well." (Group 4) Some resorted to self-help remedies with little evidence of success; sometimes even resorted to harmful practices, for example, burning vinegar and herbal medications. "My auntie bought some vinegar to boil and perfume the house." (Group 3) "A Chinese herbal store sold a herbal tea that was said to prevent SARS, then each of the family members, consumed 10 sachets during mealtime, so the whole car was fully packed (with herbal tea sachets)." (Group 6) "I wondered whether Chinese medicine would be more effective... If I was really that unlucky, I would try to use Chinese medicine to treat me instead of taking ribavirin and steroids as prescribed in Hong Kong."(Group 6) 6. Communication and education Our sampled parents believed the government officials of Hong Kong and China were hiding vital information from them. People generally felt the governments had a poor sense of surveillance and prevention of the disease and that they were totally unprepared for the epidemic. They saw numerous flaws in the existing health care policies and health care system, and perceived that the government was incapable of dealing with an epidemic outbreak. Communications among the government departments and frontline workers often appeared confusing and poor. When the government finally acknowledged the outbreak in the community, the response was regarded as 'slow, inappropriate, and inadequate', and our informants had already lost their confidence in the government. "The Chinese government officials hid information from the people, they did not tell the whole truth, thus, I only believed half of the information they gave." (Group 1) "Their (the governments') transparency was not high. And even at the very beginning, they had a poor sense of awareness." (Group 3) Another major criticism from the public was regarding the quarantine policy. This policy created tension between human rights and the social good. Some people felt a suspected case would invariably become a definite case of SARS if the patient was kept in the hospital. Parents would be particularly concerned if their children were sick and isolated in the hospital which was perceived to be worse than "death". As one parent puts it, "Maybe once admitted, people who had no SARS will be infected with SARS. Because they (the hospital) put suspected cases and real SARS cases in the same ward, which might have led to cross infection." (Group 6) "It did not matter that you were sick and admitted to the hospital. The most miserable of all was that you were alone- even your mother could not visit you. There was complete isolation, and no one was allowed to visit you." (Group 6) Conversely, the mass media was perceived as prompt and an effective means of communication to the public. Television, radio, newspaper, and the Internet provided intensive up-to-date information regarding SARS progression and preventive measures. Clearly, evidence-based publicity and school education can inevitably alleviate unnecessary fear and stigmatization. "At the later stage of SARS, the government had a 'hand-washing' TV announcement. Kids liked to watch TV and were affected. They became too compliant and washed hands frequently." (Group 3) "The school is a very important media for the education of children. Usually, kids would not listen to what we (parents) say, but they would listen to their teachers." (Group 2) Discussion The fear that originated from the uncertainties of a new emerging disease as well as the guilt of spreading the disease to others were the key concerns among the public during and one year after the SARS epidemic in Hong Kong. In response to this fear and panic, parents of kindergarten pupils acted differently; some actions were rational (from a public health prospective) but others were irrational. Rational behavioural changes such as adopting a healthy lifestyle or improving personal hygiene might enhance self-control and attenuated fear, whereas many irrational ones such as blaming other groups and boiling vinegar could potentially intensify the fear. Inappropriate changes in health-seeking behaviour and self-imposed isolation interacted with stigmatization were found to be the most prominent avoidance behaviours in SARS. These should have been alleviated by improved communication and education. The Fear Cycle (Figure 1) was thus created to summarize the above social phenomena observed at the time of a newly emerging epidemic. In this cycle, we have highlighted the role of better self-discipline, which may help mitigate fear and assist in infection control. More importantly, a persistently positive lifestyle change is not only beneficial to infection control but is also an invaluable asset in the overall health quality improvement of the population. Some of the findings in this study are consistent with those of the CDC model.5 However, more variables were found to contribute to the momentum of fear than previously identified including treatment, trust and communication of the government or health professionals, perceived government health policy, the risk communication of the mass media, and education.
There are, however, several limitations to this study. The kindergartens selected were restricted to one district of Hong Kong. Our sampled area might have had relatively more psychological burden and awareness of SARS prevention as the Prince of Wales Hospital (where the first SARS case in Hong Kong was found) is situated in this district. In fact, a large number of health care workers and their families worked and lived in this district. It was also noticed that most of the informants were females (90%). This reflected that the mothers were the main caregivers of their children and they probably had more time to participate in parental meetings than the fathers, thus potentially a problem of self-selection bias and generalizations must be made with caution. In addition, interviews were conducted one year after the SARS outbreak and there may have been a recall bias, but this drawback could be balanced by the significance and meaning of events that remained in their memory. The SARS epidemic undoubtedly caused tremendous social destruction and disruption. However, from another angle, the outbreak provided an opportunity to expose the deficiencies of the existing health care system, and served as a stimulus to improvement. It is important to understand the rationale behind people's fear as an integrating step when formulating policies on the prevention and management of any newly emerging disease. As demonstrated in the Fear Cycle, there are multiple points available for intervention using the behaviour intervention approach. Efforts should be focused on encouraging and sustaining rational behaviours such as better hygiene and self-discipline while demystifying discrimination and stigmatization that associated with diseases and compulsory preventive measures such as quarantine. This can be achieved by better risk management such as educating the general public on measures of controlling infectious diseases, for instance, in undergoing quarantine (who should submit to it and how it is decided) and the quality of care one may receive well in advance of any expected outbreak. For example, the Hong Kong Hospital Authority has prepared a detailed guideline to manage the potential pandemic outbreak of avian flu, but little of its contents have been conveyed to the general public. A patient-centered approach should be adopted by the health professionals. In any newly emerging disease of many unknown characteristics, patients and their relatives should be fully engaged when deciding on treatment options and throughout the treatment of the disease. The mass media also has a significant role to play. Early and appropriate use of mass media to communicate with the public will certainly be beneficial. However, doctors must be cautious when interacting with the media and should try to check the accuracy of its content for which they have been interviewed before they are printed.18 Hotlines manned by trained professionals and modern communication technology such as the Internet or short-text messages through mobile phones can be implemented and monitored at the early stage of an outbreak. In the case of our targeted population (parents and young children), specific instructions regarding schooling, childcare arrangements and in-patient service for parents or siblings should be considered and discussed among concerned groups. There is no funding support for this project. The authors do not have any known conflicts of interests regarding this manuscript. Ethics committee approval was obtained from the Survey and Behavioural Subcommittee, The Chinese University of Hong Kong. Key messages
William C W Wong, MBChB (Edin), MA (Dist), MMFTM RCPS (Glasg), MRCGP (UK)
Assistant Professor, Department of Community and Family Medicine, The Chinese University of Hong Kong. King-chi ChanKing-chi Chan, LMCHK, MFM (CUHK) Medical Officer, Shek Wu Hui Jockey Club Clinic. Hiu-wai Tang, LMCHK, MFM (CUHK) Medical Officer, Tsing Yi Town Clinic. Michael W H Lam, Medical Student Flinders University School of Medicine, Australia. Correspondence to : Dr William C W Wong, Department of Community and Family Medicine, The Chinese University of Hong Kong, School of Public Health, Shatin, NT, Hong Kong.
References
|
|