|
August 2003, Volume 25, No. 8
|
Original Articles
|
Transferrin saturation for the diagnosis of iron deficiency in febrile anaemic childrenC H Li 李澤荷, A C W Lee 李志偉, T W L Mak 麥永禮, S C Szeto 司徒紹昌 HK Pract 2003;25:363-366 Summary
Objective: To study the sensitivity of commonly used laboratory
markers in the diagnosis of iron deficiency anaemia (IDA) in children found incidentally
to be anaemic during hospitalisation.
Keywords: Anaemia, Children, Ferritin, Iron deficiency anaemia, Transferrin saturation 摘要
目的: 通過住院後意外發現患有貧血的兒童進行缺鐵性貧血(IDA)診斷,研究相應常用實驗室指標的敏感性。
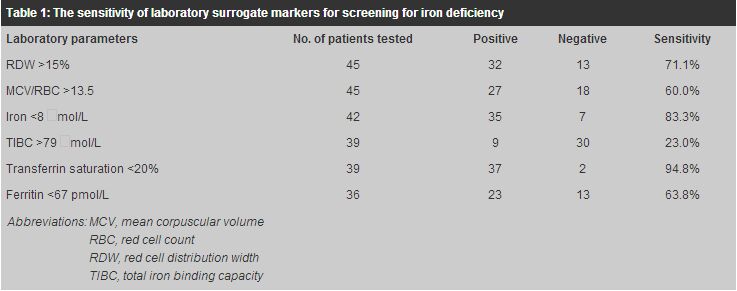
Introduction Iron deficiency is the commonest nutritional deficiency in the world and constitutes a major health problem in children, even in developed regions.1 The clinical manifestations of iron deficiency anaemia (IDA) can be subtle, and significant psychomotor retardation may occur in the young child if iron deficiency is severe and prolonged.2 Definitive diagnosis of iron deficiency relies on the demonstration of depletion of iron reserves in the body; for example, the absence of stainable iron in the bone marrow.3 However, bone marrow aspiration is an invasive procedure and is not recommended for routine diagnosis.4 Instead, a number of biochemical and haematological parameters including ferritin, transferrin saturation, total iron binding capacity (TIBC), and red cell distribution width (RDW), have been used as surrogate markers for iron deficiency and hence initiation of iron supplementation.4,5 Under such circumstances, the ultimate diagnosis of IDA rests on the correction of anaemia after adequate treatment.2 These biochemical and haematological surrogate markers of iron deficiency are often used in combination clinically, but their relative merits for the recognition of IDA are unclear. In clinical practice, where anaemia is often detected "incidentally" during the management of acute infectious disorders, the reliability of biochemical markers has been queried.6 This retrospective study was carried out in order to assess the sensitivity of a number of commonly used laboratory parameters as markers of IDA. Methods The study was carried out in the paediatric unit of an acute general hospital, where children under the age of 16 years were admitted. The management of anaemia (haemoglobin <11g/dL) found during the course of hospitalisation has been previously described.7 In brief, the affected children were offered the following tests: full blood counts, serum iron, TIBC, transferrin saturation (serum iron/TIBC x 100%), serum ferritin, and haemoglobin electrophoresis. The patients were also offered a 4-week course of iron therapy, after which they would return for follow-up of their initial laboratory findings and a repeat measurement of haemoglobin.
This is a retrospective hospital chart review of all children who were diagnosed
with IDA between July 1999 and June 2001. The WHO criterion of a therapeutic response
- defined as a rise of haemoglobin by at least 1g/dL in a 4-week interval after
iron therapy (4-6mg of elemental iron/kg/day) - was used as the standard for diagnosis.2
The inclusion criterion was age between 6 months and 15 years. Children were excluded
if they had received blood transfusion, had prior history of iron treatment, or
had known chronic inflammatory illnesses. The results of the following laboratory
tests were obtained: mean corpuscular volume (MCV), red blood count (RBC), RDW,
serum iron, transferrin saturation, TIBC, and ferritin. According to the hospital
reference values, a positive test for iron deficiency was defined as RDW >15%,
serum iron <8
As there is no simple test to exclude IDA, and patients who failed iron therapy might have poor compliance or persistent blood loss, the true negative rate for IDA could not be ascertained. Hence, the specificity of the tests was not measured. Results
Forty-five children, including 21 girls and 24 boys, were diagnosed with IDA by
therapeutic response and satisfied both the inclusion and exclusion criteria. Their
mean age was 6.4 years and the mean haemoglobin at presentation was 9.3g/dL.
Discussion Iron deficiency anaemia (IDA) remains a global childhood problem.1 Its prevalence in Hong Kong has not been studied in full. An estimated 0.3-0.6% of middle school children may be affected.9,10 IDA is characterised by the presence of microcytic, hypochromic anaemia, a feature that is also shared by a number of the thalassaemic syndromes. IDA and thalassaemia may co-exist in the same patient. In areas where thalassaemic syndromes are common, the diagnosis of IDA using simple haematological parameters is difficult.6 The absence of stainable iron in a bone marrow aspirate provides a definitive diagnosis of IDA, but the procedure is too invasive for routine clinical use. Hence, a number of biochemical tests and haematological parameters have been recommended for the indirect diagnosis of IDA. The diagnosis can be confirmed by the correction of anaemia after adequate iron treatment.2 The interpretation of these biochemical markers may be difficult in clinical practice where anaemia is often evaluated amidst acute febrile illnesses. Serum iron represents <0.1% of the total body iron. Besides IDA, a low serum iron level may also be seen during acute or chronic infections, whereas haemolysis or liver disease may increase its measurement.11 Serum ferritin has been traditionally taken as a reliable marker of body iron stores, and hypoferritinaemia is commonly used as a diagnostic marker for iron deficiency.3 Because it is an acute phase reactant, however, a normal or raised serum ferritin level may be seen during acute infections or liver disease even in the presence of iron deficiency.12,13 An increase in TIBC is also indicative of iron deficiency, but it suffers the same drawbacks as serum iron measurements.11 It is therefore not surprising that both TIBC and serum ferritin were found to be relatively insensitive (23% and 63.8%, respectively) in detecting IDA in the present study. Transferrin saturation, an indicator of iron transport that derives from the ratio of serum iron and TIBC, appeared to be a sensitive marker of iron deficiency in our study. As the conditions affecting serum iron and TIBC levels tend to increase or decrease both measurements in the same direction,11 transferrin saturation may be more applicable in our clinical practice. Others have tried to circumvent the problem by looking at red cell indices generated by automated cell counters and derived functions from these indices for the diagnosis of iron deficiency. An RDW >15%14 or a Mentzer's index (MCV/RBC) >13.57 have been found to be useful indicators, especially in the differentiation of IDA from thalassaemic disorders. However, both parameters were not found to be sensitive indicators (sensitivities 71% and 60%, respectively) in our study. The high rate of co-existing IDA and thalassaemic traits in our study might have undermined the usefulness of these indices. It would be ideal if the specificity of these tests could be evaluated; however, in order to do this, we would need to know the true prevalence of anaemic children without iron deficiency. Unfortunately, we do not have a non-invasive and routinely available test to exclude iron deficiency. Failure to respond to iron therapy cannot be taken as exclusion for IDA because poor drug compliance or ongoing blood loss might be the underlying cause. From a clinical point of view, however, the specificity of the test is not important as long as the test is sensitive enough to select the appropriate patients for iron treatment. Our findings also allow us to assess the feasibility of cost saving in the evaluation of IDA in children. The combined tests of serum iron, TIBC, and serum ferritin cost HK$35 of which serum ferritin alone costs $30. Eliminating the routine use of serum ferritin measurement means that the cost can be reduced by 86% per patient tested. Conclusion The study confirms that the use and interpretation of biochemical markers and red cell indices in the evaluation of suspected IDA in children presenting with febrile illnesses should be viewed with caution. For the investigation of the commonly encountered microcytic, hypochromic anaemias, the use of transferrin saturation alone in addition to haemoglobin electrophoresis (c.f. thalassaemic disorders) may represent the most sensitive and cost-effective combination of tests. Key messages
Y T Wun, MBBS, MPhil, MD, FHKAM(Fam Med)
Member,Research Committee, The Hong Kong College of Family Physicians,Formerly, Department of Community and Family Medicine, The Chinese University of Hong Kong. T P Lam, MBBS(W Aust), MFM(Monash), PhD(Medicine, Sydney), FRACGP Associate Professor, Family Medicine Unit, Department of Medicine, The University of Hong Kong. L C Y Tsang, MBBS, DFM(CUHK), FRACGP, FHKAM(Fam Med) Consultant Family Physician, Training Centre in Family Medicine, Department of Health, Hong Kong SAR. Correspondence to : Dr Y T Wun, Research Committee, HKCFP, Room 701, HKAM Jockey Club Building, 99 Wong Chuk Hang Road, Aberdeen, Hong Kong.
References
|
|