|
March 2001, Volume 23, No. 3
|
Update Articles
|
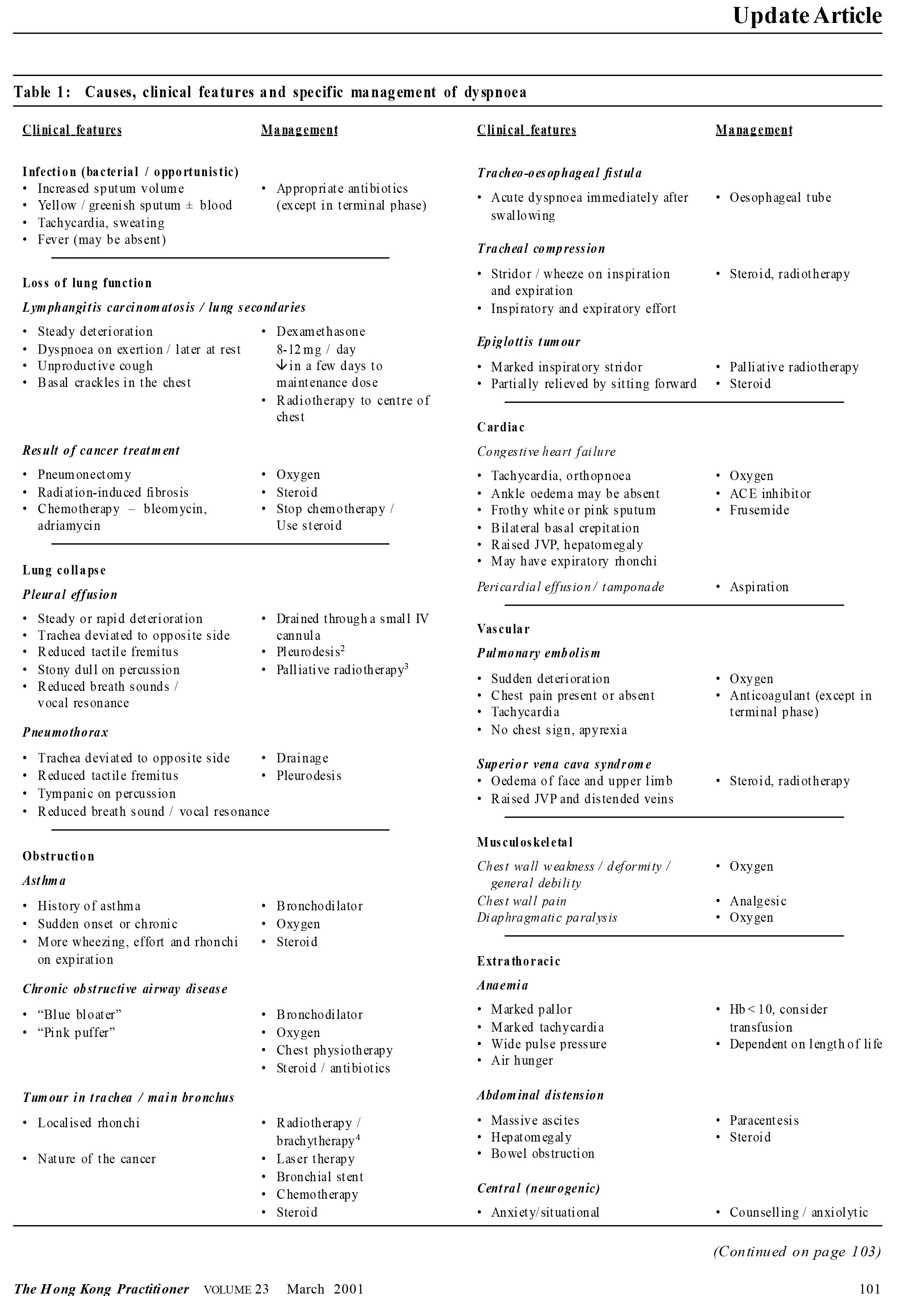
Dyspnoea in palliative medicine*VS P Chan HK Pract 2003;25:127-133 Summary Dyspnoea, common in advanced cancer patients, has many causes. Specific treatment of the cause is more effective than non-specific treatment alone. Detailed assessment for the cause is therefore mandatory. Morphine is the drug of choice for symptomatic relief of dyspnoea. Other respiratory sedatives, such as promethazine and chlorpromazine are helpful . Anxiolytics are given to anxious patients. Oxygen is helpful in certain conditions only. Non-drug management is equally important. Refractory dyspnoea in terminal stage can be managed by heavy sedation. Introduction Dyspnoea occurs in between one quarter and three quarters of patients with advanced diseases, not only in patients with cancers of the respiratory system. It is present in 70%of patients with advanced cancer during the last six weeks of life.1 Continuous dyspnoea may be the most distressing and panicking suffering for both patient and family. Causes and clinical features Table 1 shows the causes of dyspnoea and their clinical features. Hyperventilation due to panic attack and tachypnoeawith acidotic breathing in acidosismaymimic dyspnoea. Fatigue, fear and panic also exacerbate dyspnoea. Cachexia and weakness of the patient can present as dyspnoea on exertion.
Assessment A complete history and physical examination can often provide enough information formaking a diagnosis. History Ask for the nature, severity and duration of dyspnoea. Has deterioration been rapid or slow? Take a history about the symptoms of the possible causes of dyspnoea as we would from an ordinarily dyspnoeic patient. In addition, ask in detail what treatment the patient has had for his cancer. Is the dyspnoea related to eating or drinking? Is the difficulty of breathing more severe on inspiration or expiration? How does it affect the quality of life? Assess the psychological status of the patient and carers. Physical examination Examine the patient aswe would for a non-cancer patient. Look for signs of the possible causes shown in Table 1. The patient's underlying chronic obstructive airway diseases (COAD) or asthma might have been exacerbated by some cancer related problems. Presence of ankle oedema, basal crepitations and raised jugular venous pressure do not necessarily indicate heart failure. Ankle oedema is quite common in advanced cancer patients. Basal crepitation can occur in lymphangitis carcinomatosis. Raised jugular venous pressure with the associated oedema of the face and upper limbs may be caused by obstruction of superior vena cava. There may be localised rhonchi and crackles caused by localised obstruction or compression. Look for signs of extrathoracic causes such as anaemia, uraemia and distended abdomen caused by enlarged organs, bowel obstruction or massive ascites. Look for signs of anxiety and panic disorder. Investigation Chest x-ray helps in confirming the diagnoses of pneumonia, atelectasis, lymphangitis carcinomatosis, pleural effusion, heart failure and chronic pulmonary disease. In lymphangitis carcinomatosis, chest x-ray shows reticular markings radiating from the hilar region which may be widened by enlarged lymph nodes. Widespread or miliary markings can be due to multiple metastases, infection, haemorrhage or drug toxicity. X-ray with contrast swallow is helpful in diagnosing tracheo-oesophageal fistula which presents with cough and dyspnoea on drinking and eating. Laryngoscopy and bronchoscopy may be done for suspicion of laryngeal growth with st ridor and tracheobronchial compression or obstruction. Stent insertion or laser treatment may be done at the same time if indicated. Ful l blood count, sputum cult ure, CT scan, spirometry, blood gas and ventilation-perfusion scanning may also be done if indicated. Management Treat the cause if possible. Table 1 also shows the specific treatment for the various causes of dyspnoea. Apart from these, there are some non-specificmethods for relieving dyspnoea. Specific management The rationale of some specific management shown in the table is obvious and similar to the management of the condition in non-malignant patients. Pleurodesis after drainage of pleural effusion in malignant condition is effective in retarding recurrence of effusion with dyspnoea.2 Small cell carcinoma of the lung is highly responsive to chemotherapy. Combination chemotherapy in non-small cell lung cancer has resulted in symptom relief,5,6 and increase in median survival by 6-8 weeks compared to untreated patients.7-9 Radiotherapy gives effective palliation of symptomswith minimal side-effect to non-small cell carcinoma of the lung, but there is no evidence that it can prolong survival.10 Stenting and/or laser resection of endobronchial tumour are effective in controlling dyspnoea. Antibiotic is the choice of treatment for bacterial chest infection. However, its use may not be indicated in terminally ill patients. Similarly, whether to treat pulmonary embolism with anticoagulants also depends on the stage of the disease. The patient and family should be involved in decision making. Non-specific management The patient is less dyspnoeic if the need for exertion is reduced, such as using home-helper and using wheelchair and bedside commode.11 The patient can be propped up with pillow or sleep in a chair. He can be distracted by reading or watching television. Although stopping smoking is too late to prevent cancer, smoking can exacerbate dyspnoea. Open the window and use an electric fan for facial cooling can relieve sensation of dyspnoea through stimulation of the receptors of the trigeminal nerve. Physiotherapist can teach the patient to do breathing exercise, deep breathing and coughing. He can also do the postural drainage of retained secretion, percussion, vibration and suction. Humidified air from steam or nebul ised sali ne and mucolyt ic agents such as acetylcysteine or bromhexine can loose tenacious sputum.1 Excessive secretion in the terminal stage can be reduced by anticholinergic drugs. Wheezing caused by reactive bronchospasm in congestive heart failure, retained secretions or tumour in the main bronchi can be relieved with nebulised bronchodilator. Anxious patients For panicking or anxious patients, reassure and accompany them and respond to their questions. Emphasise that breathlessness can be relieved. Becoming breathless is not dangerous and that they will not suffocate. Identify situational and psychological components. Teach them to do relaxation exercise, meditation and breathing exercise. Refer to music therapy, hypnotherapy, conventional or religious counselling. Hold the patient firmly during panic attacks. Drug management Opioids Morphine and other opioids have a direct effect on brain stemrespiratory centre.12,13 They reduce respiratory drive, alter central perception of breathlessness, decrease carotid body discharge, and reduce metabolic rate and oxygen consumption. They also sedate the panicking patient but the patient may become very drowsy if not used for pain. They can be started with 2-4mg fourhourly orally and be increased daily by 2 mg/dose until relief of dyspnoea or drowsiness occurs. It is unusual to require more than 2.5-5 mg subcutaneously or 5-10 mg orally every four hours.11 If the patient is already on morphine, it will have little benefit on dyspnoea until adequate analgesia has been achieved. The dosage can be increased by 10% increments beyond the painmanagement dosage. It may need to be increased up to 50% more than the original dosage. At this dosage, drowsiness is inevitable. Morphine solution for injection can be administered via a nebuliser in the dosage of 10-40 mg up to three hourly.14 However, it may cause bronchospasm and its effect has not been supported by clinical trials. So, if it is used as a last resort, bronchodilator inhaler or nebulising solution should be readily available and the dosage should be titrated upward from a low dose. Steroid Steroids can reduce peritumour oedema with improvement in obstruction. Theymay also improve lung stiffness due to parenchymal infiltration. As a result, they are indicated in obstructive dyspnoea and lymphangitis carcinomatosis where there are blockage of lymphatic drainage of the lung at the hilar lymph nodes resulting in lung stiffness and impaired oxygen diffusion through the alveoli. They are also useful for patients with acute exacerbation of chronic obstructive pulmonary disease.15 Dexamethasone can be started with 8-12 mg daily and reduced at weekly intervals to a maintenance dose of around 2-4 mg daily. Prednisone or prednisolone has more minerocorticoid side-effects than dexamethasone. Anxiolytics Benzodiazepines such as lorazepam 0.5-1mg orally or sublingually can be used for short term relief. Diazepam has a longer half-life and can be used for long term anxiety. 5-10mg can be given at bed-time orally and the dose be reduced if drowsiness occurs after several days and in elderly. Although diazepam ismuch cheaper, it has more potent depressant effect on the ventilatory response to carbon dioxide than opioids with negative changes in terms of exercise tolerance and blood gas.16 Midazolam has been recommended for panic associated with dyspnoea. It can be given subcutaneously or intravenously.17 Other drugs Other recommended respiratory sedatives are alprazolam 0.5-4.5mg/day, chlorpromazine18 10-50 mg nocte or promethazine19 12.5-25 mg every 12 hourly. Nabi lone, a cannabi noi d, at the dosage of 0.1-0.25mg twice to 4 times a day has bronchodilating effects and sedates without reducing respiratory drive. It is useful in patients with COAD and lymphangitis carcinomatosis. The local anaesthetic agents, lignocaine and bupivacaine, can be administered by nebuliser and may improve dyspnoea.14 Oxygen Most patients do not require continuous oxygenwhen there has been optimal management with morphine and anxiolytics. However, it should be available if acute dyspnoeic attacks are likely, such as in end-stage chronic airways limitation, cardiac failure or thromboembolism, or if the patient remains extremely anxious despite efforts to counsel and control symptoms. Oxygen is useful inCOAD, congestive heart failure, recurrent pulmonary emboli, post-surgical pulmonary insufficiency and post-radiotherapy fibrosis.20 It does little to relieve dyspnoea where there is collapsed area because of shunting of deoxygenated blood. It interferes with speech, eating and mobility.21 Because it may fatally reduce hypoxic drive in COAD, it should be used in the lowest effective dose in such patients. It is administered through nasal prongs or light comfortable plastic face mask attached to nebuliser to prevent dryness. Smoking is forbidden in the patient's room. If available, use of an oxygen concentrator is cheaper. Ventilatory support is rarely indicated. Terminal stage Semiconscious and unconscious patients who still appear dyspnoeic in the terminal phase can be treated with continuous morphine infusion. Relief of dyspnoea is more important than respiratory depression or sedation.22 Restless patients can be sedated with parenteral morphine and clonazepam,midazolam or diazepam. The dosage of morphine depends on the patient's usual dose, but is usually 30mg every 4 hours or 2-3 times the dose that was being administered prior to deterioration. Clonazepam can be given 2 mg subli ngually, subcutaneously, intramuscularly or intravenously and continued with 2-4mg/24hours.Alternatively,midazolam 5-10mg can be given subcutaneously or intravenously and then continued with subcutaneous infusion at a dose of 30-90 mg/24 hours. Diazepam 10 mg can be given intravenously. The aim is to keep the patient asleep and asymptomatic. End-stage non-malignant pulmonary diseases or heart failure Intensify medicalmanagement with full investigation of the reasons for deterioration to give the patient a chance of improvement. When the patient is still distressfully dyspnoeic despitemaximal therapy, use of morphine and anxiol ytics as descri bed above is appropriate if their renal and hepatic functions are normal. Commence treatment at the lowest dose and titrate until the desired effect is achieved. These patients, afterall, deserve good quality of life made possible by quality palliative care. However, in patientswith non-malignant diseases, patient and family involvement with options and decision-making is particularly more important than in terminal cancer patients. Key messages
V S P Chan, MFM,MMe d(Pal liative Car e),FAChPM(RACP), FRCGP
Adjunct Associate Professor in Palliative Care, Faculty of Communication, Science and Health, Edith Cowan Univer sity, Wester n Australia. Correspondence to : Dr V S P Chan, 37 John Street, Cabr amatta, 2166, Austr alia.
References
|
|