|
August 2001, Volume 23, No. 8
|
Update Articles
|
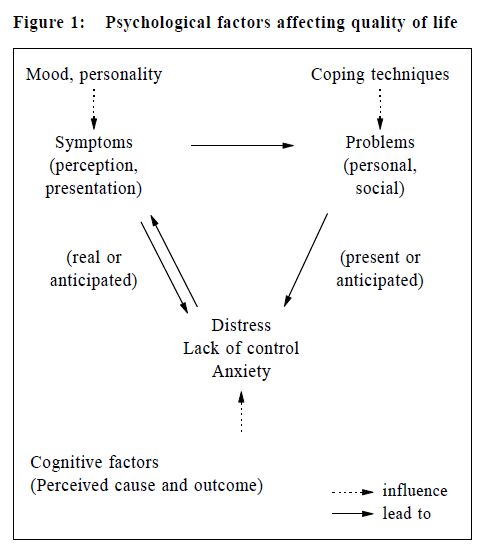
Principles of palliative medicine*V S P Chan 陳瑞波 HK Pract 2001;23:338-342 Summary Because of limited life expectancy and extent of multiple symptoms, the approach in palliative medicine is different from family medicine although there are many similarities between the two. The main goal of management is improving the quality of the patient's life through symptom control and dealing with psychosocial, spiritual and cultural factors. An interdisiplinary domiciliary service enables the patient to stay and die at home. Discussed in the paper are the general approach, communication problems, drug management and decision making process when palliative medicine is provided by family physicians. 摘要 由於末期病患者餘壽有限及有多種病癥,雖然紓 緩醫學與家庭醫學有不少相似之處,但兩者的處理方 法有所差別。治療的主要目的,是透過病癥控制及處 理心理、社會、精神和文化方面的問題,改善病人的 生活質素。跨部門的家訪式服務容許病人在家中接受 治療和離世。本文討論家庭醫生在提供紓緩醫療時採 取的處理方法、面對的溝通困難、用藥方法,以及作 出決定的過程。 Introduction Palliative Care was defined by World Health Organisation as "the active total care of patients at a time when their disease is no longer responsive to curative treatment and control of pain and other symptoms, and of psychological, social and spiritual problems are paramount. It affirms life and regards dying as a normal process. It neither hastens nor postpones death,emphasises relief from pain and other distressing symptoms, integrates the physical, psychological and spiritual aspects of patient care. It offers a support system to help patients live as actively as possible until death and to help the family cope during the patient's illness and in bereavement. The overall goal is the highest possible quality of life for the patient and family".1 Palliative care can be provided in the early stage of a malignancy and in a chronic non-malignant condition. It should not be restricted to patients close to death. Many physical and non-physical problems in palliative care can often be anticipated and in some instances prevented. Failure to anticipate problems is a common source of dissatisfaction for patients.2 Identification of risk factors allows planning of care. Symptom control Near perfect symptom control is the mainstay of management. The motto "To relieve often, to comfort always and to prevent hopefully" is particularly true in palliative care. It is not always possible to completely relieve symptoms. There may only be a compromise between the presence of symptoms and adverse effects from medicine.3 It is hard for us to accept this sort of suboptimum relief and to acknowledge our limitations. Yet the patient and family will treasure our commitment and not abandoning them. Each symptom has physical, psychological, social and spiritual factors. Inadequate psychosocial and spiritual care can exacerbate existing symptoms or cause new symptoms, especially pain and vomiting.4 Side effects of treatment may cause additional symptoms, e.g. dry mouth from anticholinergics, nausea and constipation from opiates, insomnia from steroids, sore mouth and dysphagia from candida infection secondary to the use of antibiotics or anticholinergics.4 Each patient may have many symptoms. Each symptom interplays with other symptoms. However, patients and families may be afraid of complaining too much. They should be encouraged to describe fully their symptoms, feelings, needs, problems and both physical and psychological sufferings. Ask specifically for constipation, diarrhoea and incontinence that are embarrassing for the patient to disclose. Physical examination Physical examination helps in making a definite diagnosis or the mechanism of the symptoms, with which a more specific and more effective management can be given. Always look into the patient's mouth because oral thrush is quite common in immuno-compromised patients. Proper management of oral thrush and dry mouth can improve appetite, reduce nausea, mouth ulcer and sore mouth. Examine the abdomen for organomegaly, ascites and intestinal obstruction as well as the fundi for signs of increased intracranial pressure in patients presenting with vomiting. Perform a digital rectal examination if faecal impaction is suspected to be the cause of constipation or diarrhoea. Patients suspected of having spinal cord compression should have a neurological examination of the lower limbs as well as an examination of the urinary and anal sphincters. Extent of dehydration, anaemia, jaundice, oedema, confusion, dyspnoea should be noted regularly and documented. These, as well as the subjective feelings such as pain, can be documented by means of numerical scale or visual analogue scale. Examine the common sites of pressure sore such as the sacral region, both greater trochanters, lateral malleoli and the heels. Psychological examination must be done in every consultation. Depression is more common than in nonpalliative care practice. Assess whether the patient and the family is pathologically sad, angry or withdrawn. Is there any denial and ambivalence adversely affecting proper management of the patient. Investigation Investigation is done only when the result is useful for decision making. The extent of investigation also depends on the life expectancy of the patient. Full blood count is useful in pale dyspnoeic patients and in patients who have had chemotherapy. Correction of anaemia and low platelets can improve the quality of life. Hypercalcaemia, a disabling but reversible condition, is not uncommon, especially in certain types of cancer. Look for it in patients with nausea, dehydration, constipation, polyuria and confusion. Chest x-ray can be ordered for reasonably well patients with suspected pneumonia. It will be wrong to decide that antibiotics would be withheld even if the patient has pneumonia. Serum albumin is usually not ordered for patients with bilateral ankle oedema because albumen is usually not given for hypoalbuminaemia. Management Goal of management The ultimate goal is the highest possible quality of life for both the patient and the family (add life to days), and may also prolong life (add days to life). Give treatment if the intended effect is for symptom control even though the side effect may shorten life, e.g. use of morphine in chronic bronchitic patient may result in pneumonia or respiratory failure (Principle of Double Effect). Withhold or withdraw treatment to allow the patient to continue the natural dying process if the treatment is futile for the patient as compared with its expected benefits. Withholding or withdrawal of treatment is not equal to euthanasia that actively and deliberately shortens the patient's life. It is impossible to assess the quality of another person's life, or the value of that life to him or her.5 Figure 1 shows the relationship between the three factors affecting the quality of life, which are the perception of symptoms, occurrence of problems and feeling of distress as well as the psychological factors that can influence them.
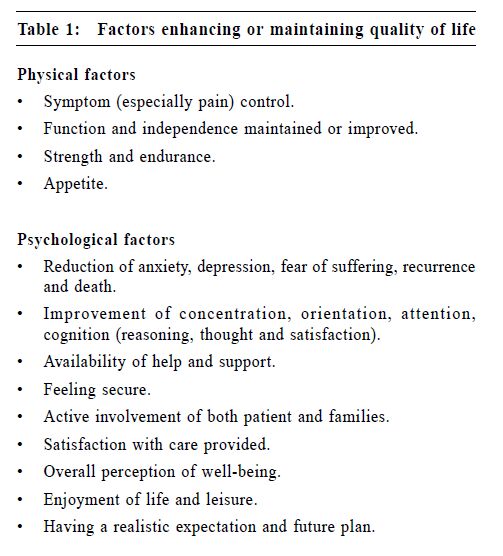
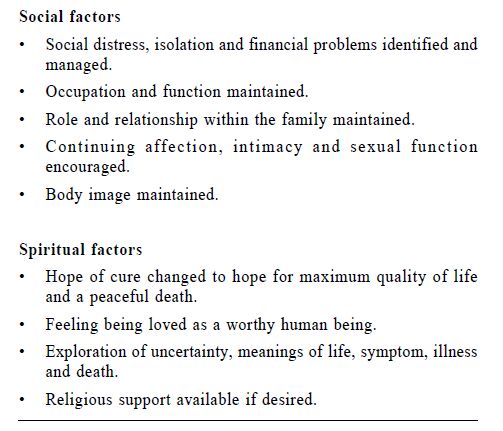
The quality of life can be improved by minimising the gap between the patient's expectations and aspirations and their actual experiences.6 Apart from physical symptom control, equally important are information, psychosocial and spiritual support as well as enhancement of coping capabilities. Table 1 shows the factors that enhance or maintain the quality of life.
General approach Our aim is to help the patients live with cancer (not die of cancer) and prepare for death while retaining their individuality, dignity and self-respect to the end. It is easier to achieve this by breaking it into a series of more achievable mini-goals that are individualised for the patients and their families. These goals are liable to sudden changes according to their changing expectations and priorities. Make a problem list. Get a full picture of each symptom. Try to understand the mechanism of each symptom and provide the appropriate treatment. Balance the benefits of treatment against the potential cost and adverse effects. Some therapeutic interventions, or even oxygen and fluid, sometimes only prolong the distress of dying. Sometimes, non-drug management can be more helpful than drug treatment. Continually review the clinical situation in the face of constant change. Many problems can be anticipated. Warn the patient and family. Have a contingency plan to prevent physical and emotional crises. This is particularly important in home care. It is important to reduce the sense of abandonment, hopelessness and despair of both the patient and family. There is always something that can be done. Be optimistic and look at the positive side such as the patients' strength and capabilities rather than their disabilities. At the same time, consider their cultural background and religious beliefs. Adopt a team approach. In practice only a few individuals will be regularly involved in any one case, the general practitioner, community nurse and specialist palliative care nurse. Yet additional allied health professionals can be called up as required. Referral to the palliative care team earlier in the disease process will give the patient and family extra support, and problems can be anticipated and prevented.7 Focus on and treat the person, not the disease. Encourage input from other team members. Care, comfort and support are always paramount. Communication Good communication skill is essential in providing good palliative care. It usually requires great thought and planning like drug prescription. Always explore the emotions of all involved. Encourage the patient and families to express and discuss their feelings. Take time to discuss. Listen carefully. Understand and empathise with their feelings and fears.8 Explanation and reassurance are as important as medication. The patient has the right to know the diagnosis and its implications. An open and honest relationship with the patient and family is itself therapeutic. Patient and family should be fully informed, honestly but tactfully, of how the disease will progress, what symptoms might occur, the rationale and purpose of investigations, the management and alternative management available (include 'no intervention'), the benefit and efficacy of all options, the types and extent of family support that is needed and available as well as the adverse effects, interactions, risks and cost of all treatment options to the family and society. The extent and pace of explanation depend on how much they would like to know and how fast they can understand and retain the relevant information. The cost includes financial cost, social cost, loss of opportunity, travel time and inconvenience to the patient and family. Give clear guidance about what to do in an emergency, whether to call the general practitioner, community and palliative care nurse or send the patient to the hospice or hospital. Tell them when to call the general practitioner if the patient dies out of hours. After the death of the patient, support the family and manage their bereavement. Physical management Management specifically aimed at the mechanism and the likely causes of any symptom is more effective.6 Catheterisation is more effective than sedation for a restless patient with urinary retention. Lowering serum calcium is import a n t f o r re l i eving nausea of hypercalcaemia. Counselling rather than taking anxiolytics is more helpful to a patient who is fear of death. A correct choice of anti-emetic specific for the pathophysiology of a patient's nausea is more effective in controlling nausea. Morphine is not a panacea. Pain of many cancer patients can be more appropriately controlled by non-opioids. Most cancer patients have multi-system dysfunction with many concurrent symptoms. Polypharmacy is almost invariable. Each symptom should be dealt with without imposing a greater burden on the patient because of intolerable, unwanted side effects or too complex a drug regimen.4 Sometimes, treatment is given immediately on preliminary diagnosis before a definite diagnosis is confirmed by investigation. Dexamethasone in high dose has to be given in patients suspected of spinal cord compression before they have radiological confirmation. Decision making Respect the decisions primarily of the patient and secondly of the family. Make sure the patient is not depressed or mentally incompetent and that they understand fully the benefits and burdens of any treatment to themselves and their family. Inform them about the available health care resources. Respect the patient as an autonomous person who can make decisions in their own best interest. Consult the family, legal guardian and the significant others. If their expectations are unrealistic, discuss sympathetically the appropriate options and the respective outcomes. Identification of possible treatments, the balancing of benefits and burdens, and the formulation of therapeutic recommendations are an integral part of a physician's responsibilities.9 The patient and family should not feel pressure from others when making decisions. Document the decisions with the reasons and the persons involved. Review decisions regularly and document them. If the patient is incompetent, his appointed advocate, closest relative or legal guardian can make decisions. Sometimes it can be hard to make decisions on whether to treat or not to treat such as giving transfusions or antibiotics and correcting electrolyte imbalance; whether to initiate tube feeding or parenteral nutrition and whether to resuscitate. Consider the possible life expectancy. There is general agreement that patients are not obliged to undergo, and doctors are not obliged to offer, begin, or maintain treatments that are futile.10 The primary goal of treatment should be maintaining the quality of life. Good decision making should include: good information exchange, informed consent, joint problem solving with patients and families as well as careful and realistic goal setting. Decisions need to be reviewed regularly as the patient's condition changes. Location of care Home care Palliative care should be delivered in the place that the patient chooses. It is possible for a patient to stay and die at home which may be most appropriate for the patient and family.11 Particular attention must be paid to their needs. Emotional and social supports and help with daily tasks are essential. Support from a team of interdisciplinary professionals and volunteers will be necessary. Equipment supply can be arranged by the community nurses or occupational therapist. Home care can be supplemented with the use of outpatient clinic and day care centre. At certain stages, the patient can still be admitted for inpatient care temporarily for respite or death. A comprehensive home service may not increase the number dying at home but enables more patients to remain at home longer.12 Day care If available, it is a good social support where patients can make new friends and enjoy cultural activities. It gives the family a break. It is also for medical and nursing care such as bathing, hairdressing, massage, dancing, craft work, physiotherapy and wound dressing. Inpatient care It is mainly for symptom management such as refractory pain and for procedures such as paracentesis or installation of spinal analgesia. It is also for respite for family and carer or for the patient to die if home death is not wanted or possible. Key messages
V S P Chan, MFM, M Med(Palliative Care), FRCGP, FAChPM(RACP)
Adjunct Associate Professor of Palliative Care, Faculty of Communication, Science and Health, Edith Cowan University, Western Australia. Correspondence to : Dr V S P Chan, 37 John Street, Cabramatta, 2166, Australia.
References
|
|